Amputation rates following limb salvage at a tertiary care podiatry centre: A retrospective analysis
Received:
Accepted:
Published:
Authors: Dr Rajesh Kesavan, Mrs Savitha Rajesh R, Dr C Sheela Sasikumar, Dr D Darwin Britto and Janani D
Citation:
Kesavan R et al (2025) Amputation rates following limb salvage at a tertiary care podiatry centre: A retrospective analysis. Global Wound Care Journal 2(1)
Declarations:
None
Acknowledgement:
We would like to express our sincere gratitude to Dr RK Diabetic Foot and Podiatry Institute’s OP & IP Department , Department of Research and Education and the Medical Records Department (MRD) for their invaluable support in data collection and patient care coordination, which made this study possible.
Corresponding author:
Dr Rajesh Kesavan, Podiatric Surgeon, Director and Founder, 1 Jayanthi Nagar Extension, Off 200 Feet Road, Kolathur, Chennai – 600 099,Tamilnadu,India drrkdiabeticfoot@gmail.com
DOI: https://doi.org/10.63896/gwcj.1.2.2
Background: Lower extremity amputation is a severe complication of diabetic foot disease, causing significant morbidity and mortality. This study reports amputation rates and post-operative quality of life following multidisciplinary limb salvage strategies at a tertiary care podiatry centre in India.
Methods: A retrospective review was conducted for all surgical admissions at Dr RK Diabetic Foot and Podiatry Institute between January 2024 and January 2025, with Institutional Ethics Committee (IEC) approval. Data included surgical admissions, amputations performed, limb salvage procedures, patient demographics, comorbidities, ulcer location, amputation level, mortality, and one-year follow-up outcomes.
Results: Among 856 surgical admissions, 821 underwent successful limb salvage and 35 required amputations, yielding an amputation rate of 4.06%. Most amputees were male (74.3%), aged 50–70 years. Below-knee amputations accounted for 74.2% of cases. Mortality was 11.1% for above-knee and 7.7% for below-knee surgeries. At one-year follow-up, quality of life assessments revealed 100% of respondents used prosthetic or assistive support; 83% retained indoor mobility, and 92% independently managed personal care. However, 29% reported emotional distress, underscoring the psychosocial burden of amputation. Follow-up compliance was 100%.
Conclusion: The low amputation rate of 4.06% highlights the effectiveness of multidisciplinary limb salvage in a tertiary care setting. Functional recovery was notable, but psychological support remains essential. Strengthened patient education and comprehensive rehabilitation may further reduce amputations and improve long-term outcomes in high-risk diabetic populations.
Lower extremity amputation remains one of the most devastating complications of diabetes mellitus and peripheral arterial disease, leading to disability, reduced quality of life, and increased mortality (Humphries, 2025; Perveen et al,2024; Barnes et al 2020 ; Setacci et al 2020)
Globally, diabetic complications result in a lower limb amputation approximately every half minute, with the vast majority of these cases linked to preceding foot ulcers. (Bilal et al, 2023)
Reducing major amputations remains a critical goal in advanced diabetic foot care. Given the chronic and complex nature of diabetic foot ulcers, a coordinated, multidisciplinary approach is essential—one that follows a staged pathway involving debridement, infection control, optimized wound bed preparation, and timely reconstruction to promote effective healing (Wang et al,2019; LK V, et al 2025) Limb salvage strategies focus on preserving functional limb integrity through a combination of infection management, vascular reconstruction, surgical debridement, advanced wound care, pressure offloading, and reconstructive surgery. (Randhawa et al, 2025)
Multidisciplinary teams have been shown to significantly reduce amputation rates, but global outcomes remain variable, particularly in low- and middle-income countries where comorbidities and resource constraints complicate care (Swaminathan et al ,2024; Adeleye et al, 2020
This study assesses amputation rates following limb salvage in a tertiary care podiatry centre in South India, offering real-world evidence on the effectiveness of coordinated multidisciplinary management.
Methods
We conducted a retrospective analysis of all patients admitted for surgical management at Dr RK Diabetic Foot and Podiatry Institute between January 2024 and January 2025. Institutional Ethics Committee (IEC) approval was obtained prior to data collection.
With IEC approval, our clinical research team extracted data from hospital records, including total surgical admissions, amputations performed, and limb salvage procedures. Additional variables included patient gender, age distribution, ulcer location, amputation level (below-knee vs. above-knee), duration of diabetes, comorbidities, mortality rates, and follow-up compliance.
Patients who underwent either an above knee (AK) or below knee (BK) amputations were monitored by the Surgical and Clinical Team for a period of two months following surgery. Prosthetic fitting was initiated after this two-month interval, with subsequent rehabilitation coordinated by the Department of Physiotherapy.
To evaluate long-term outcomes, a structured telephone survey was conducted by the Clinical Psychology team. This assessment focused on the patient’s post-operative quality of life and included targeted questions directed to both the patient and their primary caregiver.
Quality of life (QoL) was assessed using a validated questionnaire approved by the institution’s Research Committee. This tool forms part of our standard care protocol. The full set of questionnaire items is available in the supplementary materials for reference.
Limb salvage procedures encompassed:
- Surgical debridement (sharp or hydrosurgical)
- Infection control surgeries (incision and drainage, partial bone resections)
- Revascularization (endovascular angioplasty or bypass surgery)
- Reconstructive procedures (soft tissue coverage, skin grafting)
- Offloading strategies (total contact casting, custom orthoses)
- Advanced wound care (negative pressure wound therapy, bioengineered skin substitutes)
Patients were managed through a multidisciplinary team of podiatric surgeons, vascular surgeons, endocrinologists, infectious disease specialists, General Physicians and wound care nurses. Data were analysed using descriptive statistics.
Results
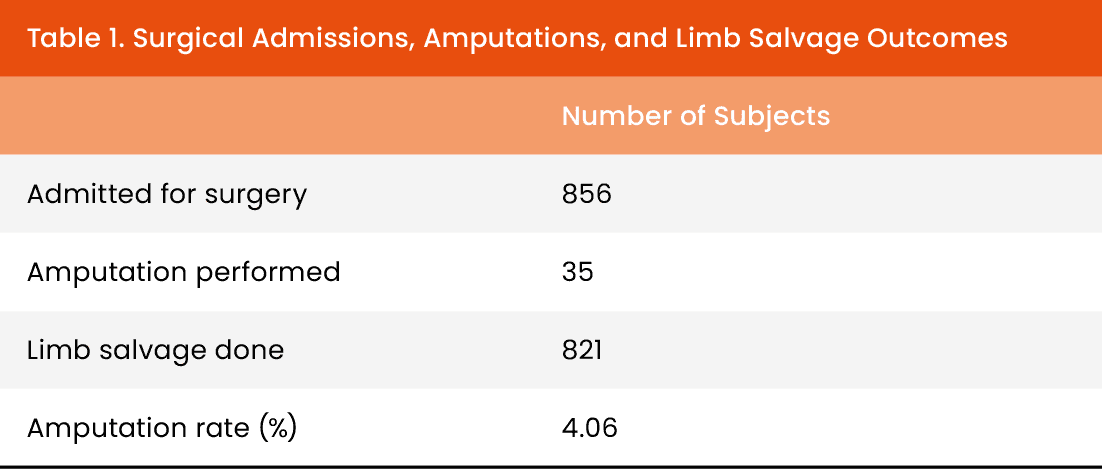
A total of 856 patients were admitted for surgical management during the study period. Of these, 821 underwent successful limb salvage procedures, while 35 required amputations, resulting in an overall amputation rate of 4.06% [Table 1]. General follow-up was conducted for all subjects, whereas the questionnaire was administered only to patients who underwent major amputations (AK and BK surgeries).
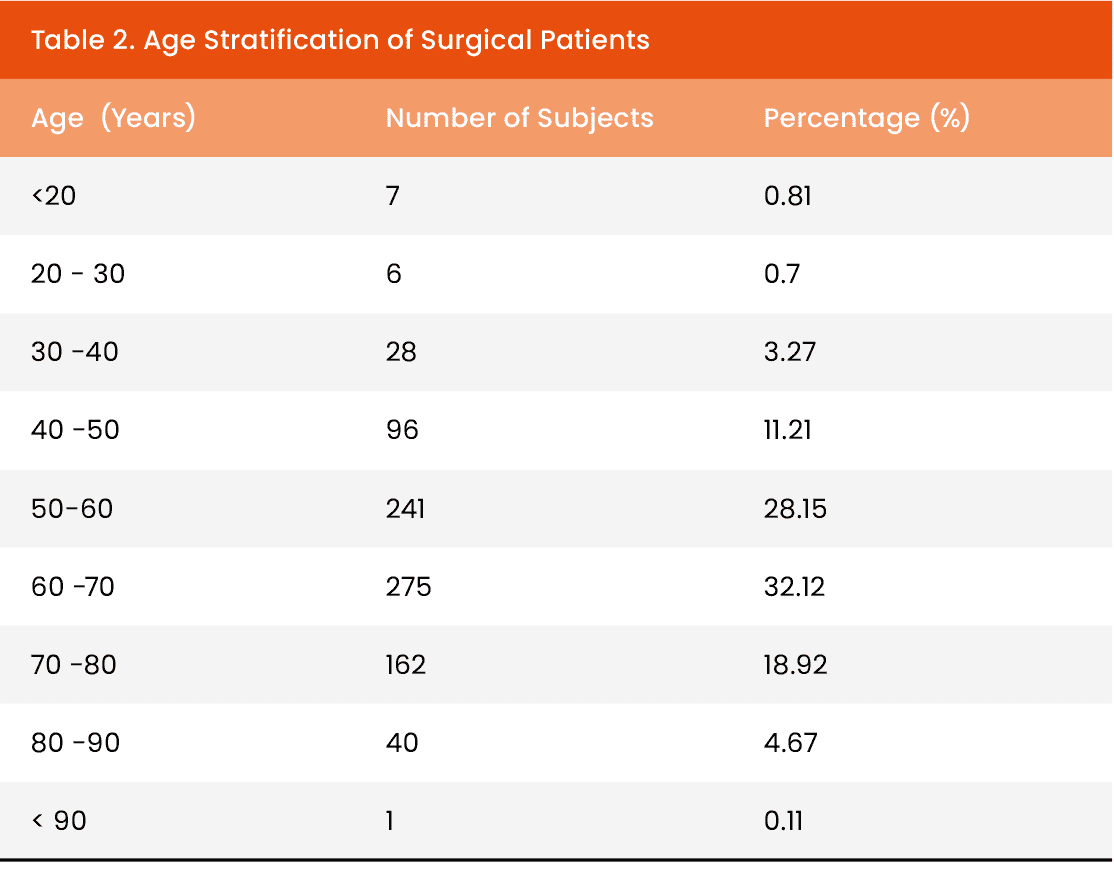
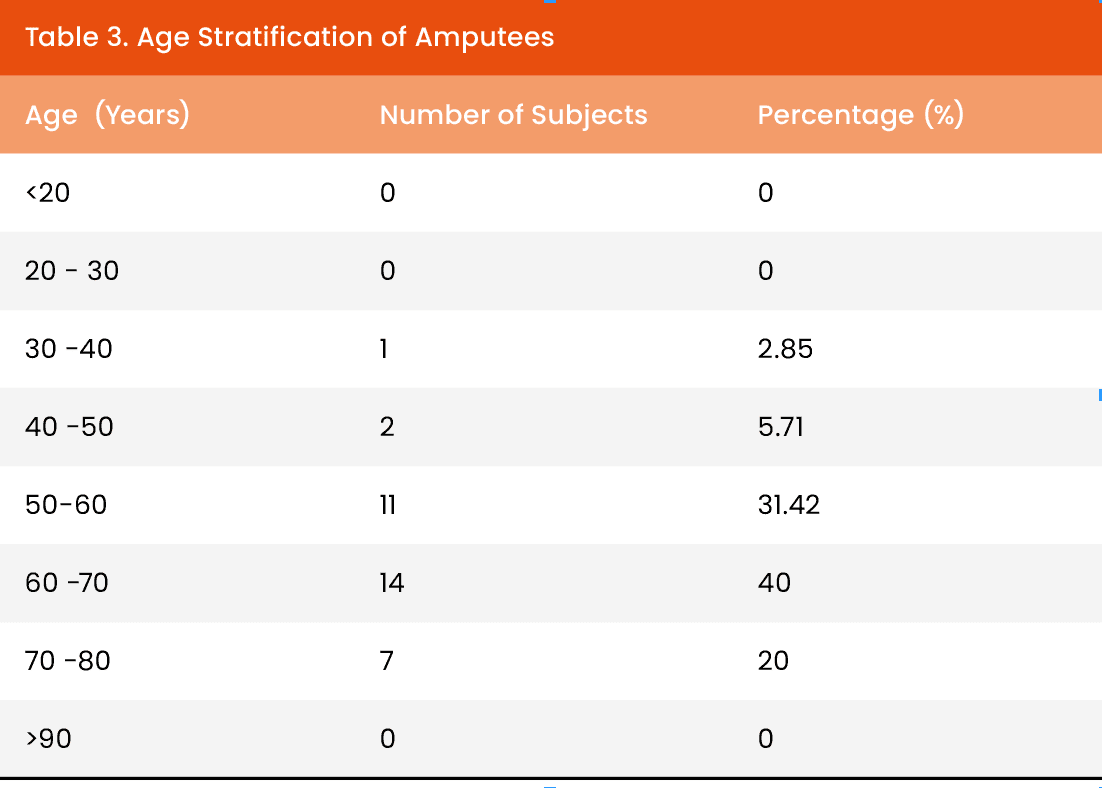
Age distribution showed most surgical patients were aged 50–70 years [Table 2]. Among amputees, the same age range dominated, with 31.42% aged 50–60 and 40% aged 60–70 [Table 3].
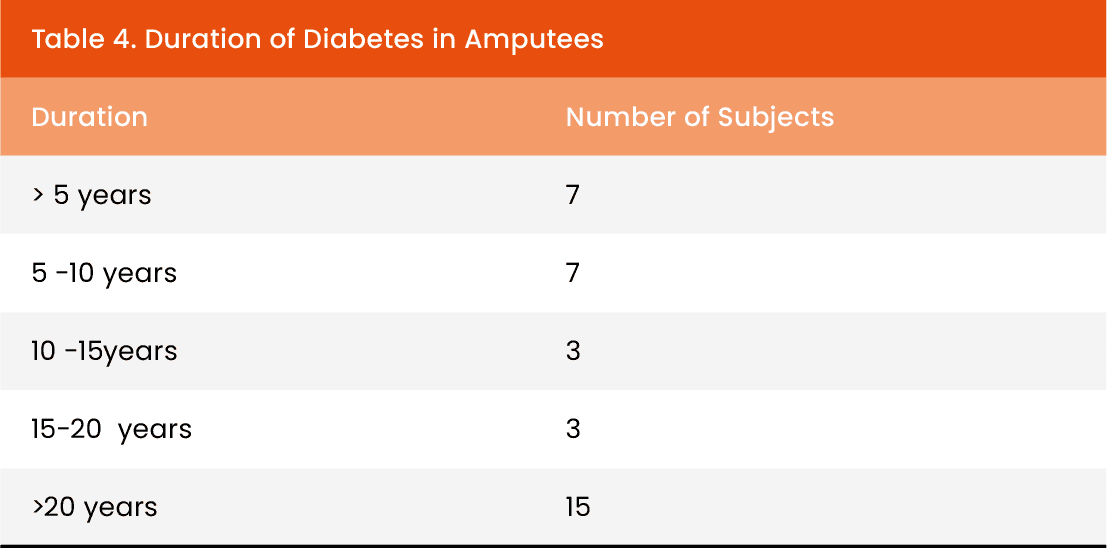
Duration of diabetes in amputees revealed a high burden of chronic disease, with 15 patients having diabetes for over 20 years [Table 4].
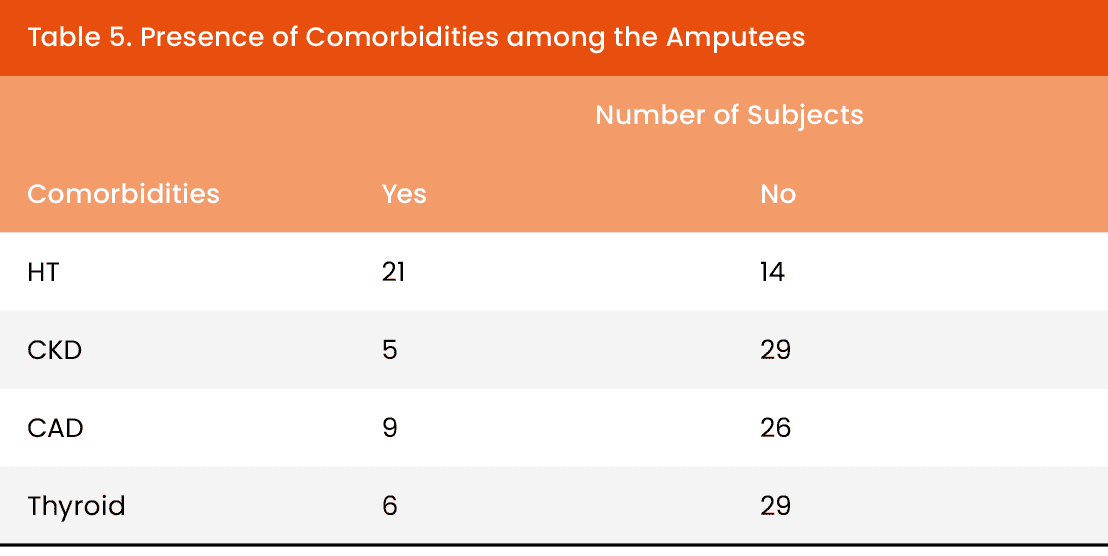
Comorbidity analysis showed hypertension in 21 amputees, chronic kidney disease in 5, coronary artery disease in 9, and thyroid disorders in 6 [Table 5].
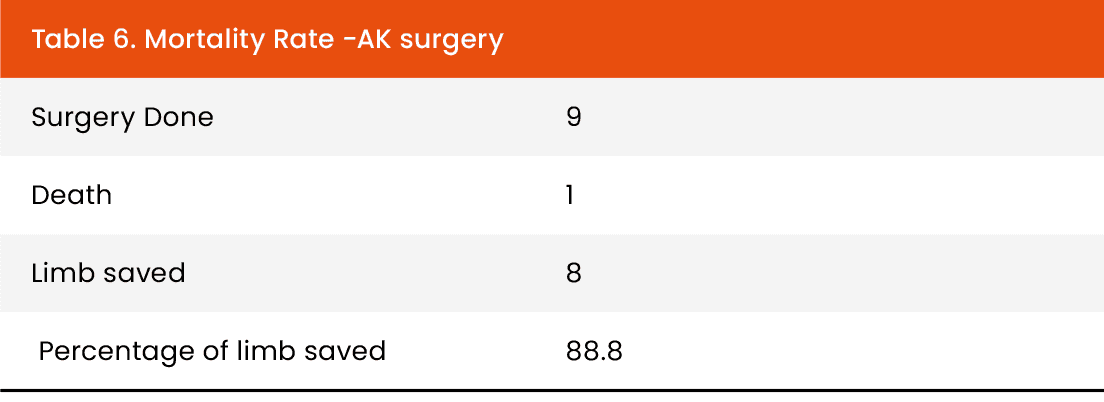
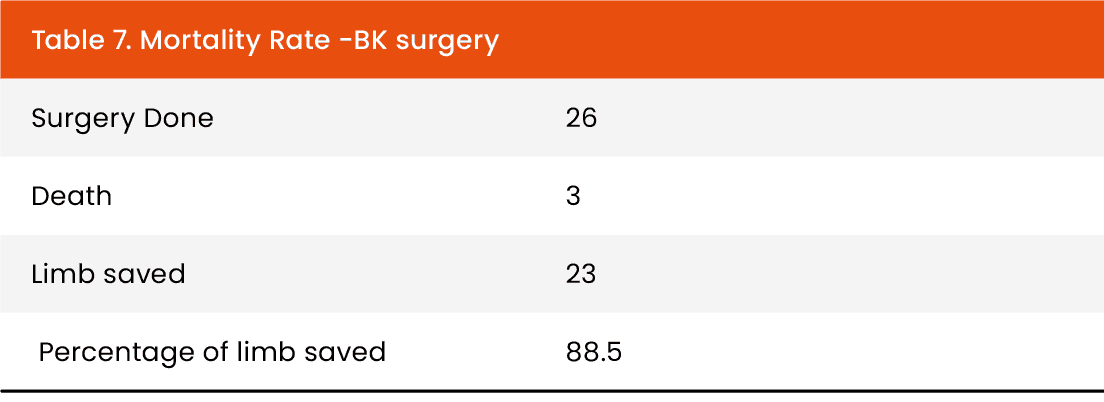
Limb salvage rate 88.5% in below-knee and 88.8% in above-knee procedures. Mortality rates were 11.1% for above-knee surgeries and 7.7% for below-knee surgeries [Tables 6 and 7].
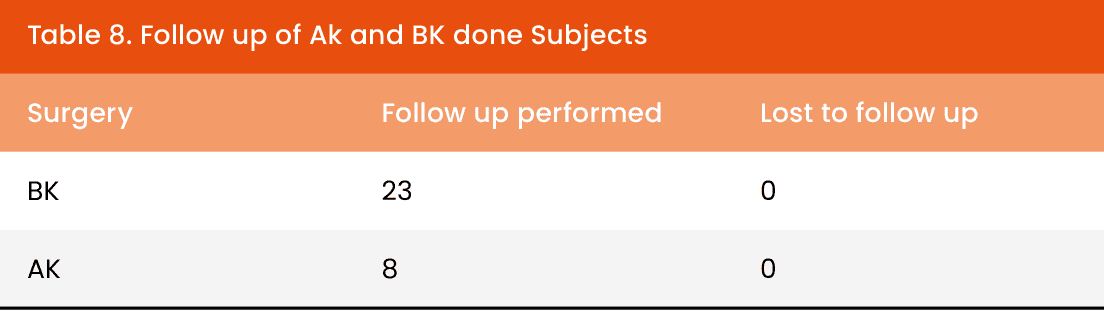
Follow-up compliance was 100%, with no patients lost to follow up. [Table 8].
Out of 31 patients who underwent above-knee (AK) or below-knee (BK) amputations:
- 24 patients (77.4%) were successfully followed up via telephonic interview at one year post-surgery.
- 4 patients (12.9%) were reported deceased.
- 3 patients (9.7%) were non-responsive despite repeated follow-up attempts.
- Quality of life (QoL) outcomes were assessed for the 24 patients across key functional and psychosocial domains: [Table 9]
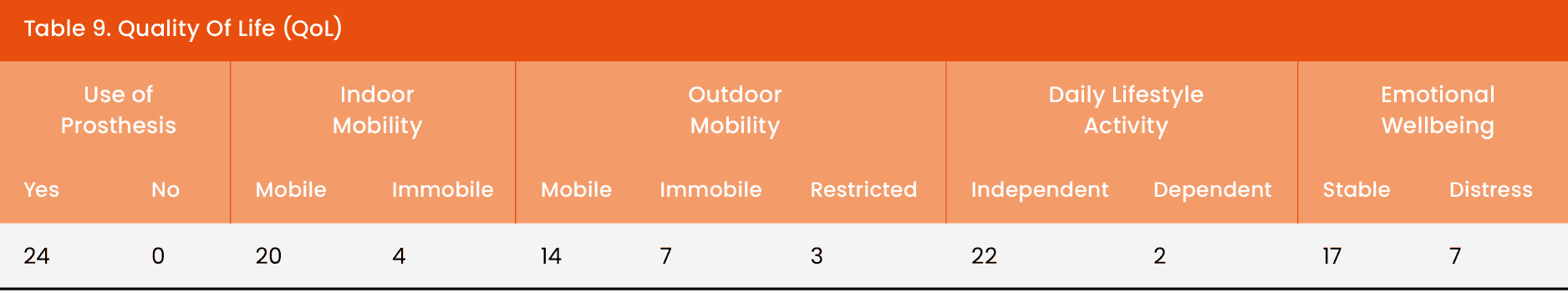
Use of Prosthetics:
- 100% (24 patients) reported using assistive support, such as walking aids or prosthetic limbs.
Indoor Mobility:
- 20 patients (83%) could move independently within their homes.
- 4 patients (17%) reported limited or no indoor mobility.
Outdoor Mobility:
- 14 patients (58%) could go outside independently.
- 7 patients (29%) were unable to go outside.
- 3 patients (13%) had restricted outdoor mobility.
Daily Living Activities:
- 22 patients (92%) managed personal care tasks (e.g., bathing, eating) independently.
- 2 patients (8%) required assistance.
Emotional Well-being:
- 17 patients (71%) reported emotional stability.
- 7 patients (29%) experienced sadness, worry, or emotional distress.
Discussion
This study found a low amputation rate of 4.06% in our tertiary care setting, supporting the effectiveness of coordinated limb salvage strategies even in a resource-constrained environment .Multidisciplinary care—incorporating infection control, revascularization, advanced wound care, and offloading—was central to these results, consistent with international guidelines (Lazzarini et al ,2023).
The higher proportion of male amputees aligns with established epidemiological patterns, highlighting the need for targeted prevention (12) (Kumar et al ,2020). In the Indian context, men are often the primary earners and are more engaged in outdoor and physically demanding activities. This increases their exposure to trauma and injuries, thereby making them more vulnerable to diabetic foot complications and subsequent amputations. The age distribution, peaking in the 50–70-year range, reflects the cumulative impact of long-standing diabetes and associated comorbidities such as peripheral arterial disease, neuropathy, and impaired wound healing. Over time, these chronic conditions compromise vascular integrity and immune response, increasing the risk of foot ulcers, infections, and ultimately, amputations in this age group. (Patil et al, 2024).
Below-knee amputations were more prevalent as per our observation (74.2% below-knee and 25.7% above-knee)as they preserve knee joint function and significantly enhance post-operative mobility and rehabilitation outcomes.. “Moreover, the lower mortality associated with below-knee amputations compared to above-knee amputations in our cohort highlights the critical importance of early detection and timely intervention in diabetic foot management. This observation is consistent with published literature. For example, in a study by Gök et al. (2016), diabetic patients with below-knee amputations had a 1-year mortality of 24.6% and 5-year mortality of 66.3%, compared to 43.3% and 83.3% respectively for above-knee amputations. (Gök et al,2016).
Our QoL outcomes demonstrate both encouraging recovery and persisting challenges in post-amputation patients. Functional results were strong, with over 80% maintaining indoor mobility and 92% performing daily living activities independently. The universal use of prosthetic or assistive devices (100%) further reflects good access to rehabilitation services. Similar findings have been reported internationally: in Nepal, Banskota et al. (2024) observed that 81% of lower-limb amputees using prostheses achieved high physical health QoL, while in Jordan, Alfatafta et al. (2025) noted that physical functioning and general health were more impaired than emotional or social domains, particularly among older individuals.(15.16) (Banskota et al, 2024, Alfatafta et al, 2025)These parallels reinforce that while indoor function and self-care are largely preserved, outdoor mobility remains a limiting factor, affecting community reintegration and independence.
Equally important, our results highlight the psychosocial dimension of recovery. Nearly one-third of patients reported emotional distress, echoing the Nepalese findings that linked mental well-being to factors such as stump pain and the level of amputation (Banskota et al., 2024). The Jordanian study also emphasized that although emotional and social functioning may be relatively preserved, impairments in physical health have downstream effects on overall QoL (Alfatafta et al., 2025). Together, these observations underscore the need for a holistic rehabilitation strategy that combines physical restoration with psychological support, enabling patients to achieve not only independence but also resilience in the long term.
Amputees must adjust to significant changes in their body’s structure, function, and appearance, which can impact them physically, socially, and emotionally. Providing effective psychological counselling before the amputation can help reduce emotional distress and alleviate anxiety about the surgery and the challenges of post-amputation life.
Providing effective psychological counselling before amputation can reduce emotional distress and alleviate anxiety about both the surgery and the challenges of post-amputation life. Counselling techniques may include cognitive-behavioural therapy (CBT) to address negative thoughts and improve coping strategies, psychoeducation to prepare patients for the physical and functional changes ahead, and supportive counselling focused on grief, loss, and adjustment. Group sessions or peer support from other amputees can also be beneficial in reducing fear of the unknown and fostering resilience.
Despite these interventions, several challenges persist. Patients often experience anticipatory grief over limb loss, fear of pain and disability, uncertainty regarding prosthetic rehabilitation, and concerns about body image, independence, and social stigma. These emotional hurdles, if not addressed, may contribute to depression, reduced motivation for rehabilitation, and poorer long-term outcomes. Therefore, structured pre-amputation psychological care should be integrated into multidisciplinary management to enhance both emotional readiness and functional recovery.
In conclusion, while physical recovery and prosthetic adaptation are encouraging, a comprehensive, patient-centered rehabilitation model is essential. This should include:
- Continued physiotherapy and mobility training
- Pain and symptom management
- Psychosocial counselling
- Community reintegration strategies
Such a holistic approach is critical to enhance both functional outcomes and emotional well-being in post-amputation patients.
Finally, perfect follow-up compliance underscores the value of dedicated post-operative surveillance and patient education. These findings suggest that even in low- and middle-income settings, robust multidisciplinary teams can achieve amputation rates comparable to high-income contexts
Conclusion
A low amputation rate of 4.06% at our tertiary care podiatry centre demonstrates the impact of comprehensive, multidisciplinary limb salvage strategies. Continued investment in coordinated care and patient education may further reduce the need for major amputations, especially among high-risk groups.
