Defining excellence in incision care: Consensus from over 100 surgeons and surgical experts on the importance of undisturbed wound healing and surgical dressing properties
Published:
Authors: Rhidian Morgan-Jones
Citation:
Morgan-Jones R (2025) Defining excellence in incision care: Consensus from over 100 surgeons and surgical experts on the importance of undisturbed wound healing and surgical dressing properties. Global Wound Care Journal 1(2): 34–40
Declarations:
The consensus meetings upon which this article draws were funded by Mölnlycke Health Care.
Statement:
No ethics and governance approvals were required, as this work is based on consensus meetings of international wound care experts. Consensus meeting participants consented to production of written reports and publications.
Acknowledgements:
The contribution of the international experts who attended the consensus meetings and the financial support from Mölnlycke Healthcare are gratefully acknowledged.
Corresponding author:
Rhidian Morgan-Jones, Cardiff & Vale Orthopaedic Centre (CAVOC), University Hospital Llandough, Cardiff, UK. Email address: rhidianmj@hotmail.com
This article synthesises the findings of 12 reports from international consensus meetings of surgical experts, held between 2019 and 2025, focusing on best practices for post-surgical incision care and dressing selection. Experts identified the importance of protecting surgical incisions, minimising disturbance and supporting healing. There was strong consensus across all regions regarding the importance of undisturbed wound healing for surgical incisions, with experts advocating dressing changes for these wounds only when clinically necessary. Characteristics of an “ideal” dressing for surgical incisions, for which there was consensus in all regions, were that it is: flexible and comfortable; fixes well to the skin; absorbent; skin-protective; waterproof and eliminates ‘dead space’ between the wound bed and dressing, with additional characteristics, such as, ease of use, promotion of healing, prevention of infection, cost-effectiveness and scarring reduction, also being identified in some regions. Regional differences and considerations (e.g. climate, geography and availability of resources), as well as wound location and individual patient needs, were considered. Consistent care, education and standardisation of practice were highlighted as essential for improving patient outcomes globally.
Over 300 million surgical procedures are undertaken across the world each year (Gillespie et al, 2021), making post-surgical incision care, including selection of wound dressings, a globally important issue with significant implications for patient outcomes.
Postoperative wounds are susceptible to a number of problems, collectively termed “surgical wound complications” (SWCs), including (Sandy-Hodgetts and Morgan-Jones, 2020):
- Surgical site infection (SSI)
- Surgical wound dehiscence (SWD)
- Hypergranulation
- Maceration of skin around the wound (periwound maceration)
- Scarring
- Medical adhesive-related surgical injury (MARSI).
SSIs are among the most common SWCs and are one of the most common causes of healthcare-associated infections (HAIs) globally (European Centre for Disease Prevention and Control [ECDC], 2023) – although up to 50% of SSIs may be preventable (Umschied et al, 2011). From a meta-analysis of nearly half a million general surgical cases worldwide, Gillespie et al (2021) estimated that 11% of incisions developed an SSI within 30 days. Reported SSI rates vary widely between countries and geographical regions (e.g. Europe 0.6–9.5% [ECDC, 2023]; Japan 1–2.1% [JANIS, 2023]; Saudi Arabia [single-site prevalence study] 10.2% [Ali Alsareii, 2021]) – and are likely to be under-estimated, due to reporting issues (WUWHS, 2018). SSI rates also differ according to the type of surgical procedure and related need for this – for example, an SSI rate of over 30% is seen for abdominoplasty in people with obesity and SSIs develop in up to 50% of surgeries for complicated limb traumas (Sandy-Hodgetts et al, 2022).
SWCs are an important global concern for a number of reasons: negative impacts – sometimes long-lasting – on patients’ physical and mental health; delayed postoperative recovery; increased length of hospital stay; high financial costs; increased need for use of antibiotics – of concern in an era of increasing antimicrobial resistance – and risk of death, with 3% of surgical patients dying from an SSI (Allegranzi et al, 2011; Rickard et al, 2020; Gillespie et al, 2021; Sandy-Hodgetts et al, 2022).
Therefore, the need for all those involved in post-surgical incision care to focus on reducing the risk of SWCs has been highlighted (Morgan-Jones et al, 2019; Sandy-Hodgetts et al, 2017, 2018).
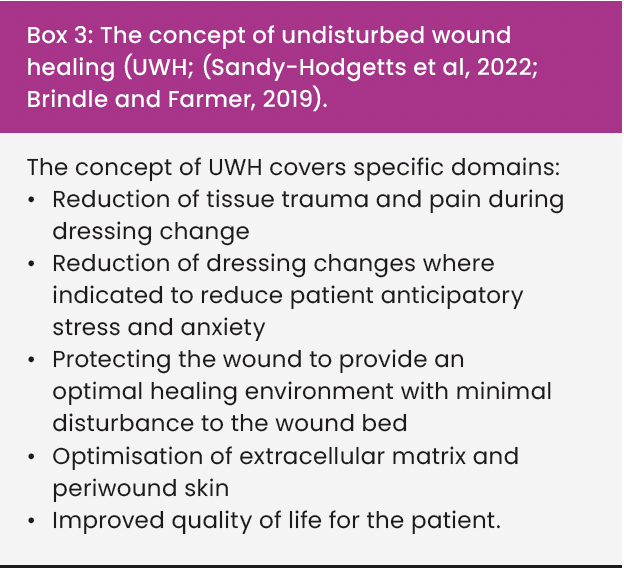
Undisturbed wound healing (UWH) has been highlighted as a key concept of particular relevance to post-surgical wounds, as it protects wounds from potential contamination (WUWHS, 2016).
Methods
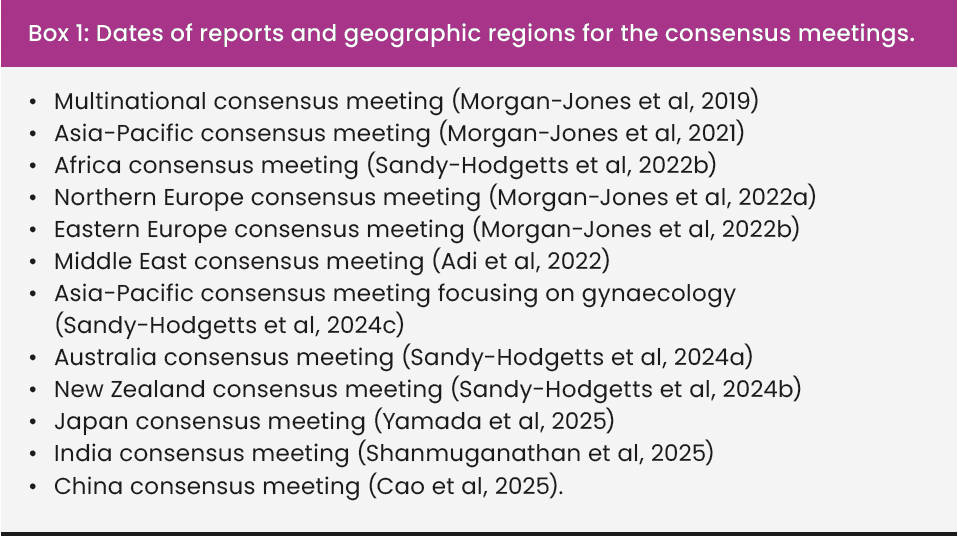
This article synthesises findings of 12 reports from international consensus meetings of surgical experts, held between 2019 and 2025. Box 1 lists the dates of the reports and the geographical regions in which the consensus meetings were undertaken; as can be seen, there was representation from a wide range of regions, facilitating development of global consensus. In total, over 100 surgeons and surgical experts contributed to the consensus meetings.
The objectives of the consensus meetings were:
- To clarify local and global views on incision care and dressing selection in surgical wounds
- To discuss key areas and reach consensus on recommendations
- To agree on the properties of the “ideal” dressing for managing surgical incisions.
Each consensus meeting involved structured discussions, facilitated by either one or two meeting chairs, focusing on best practices for post-surgical incision care, the characteristics of an ‘ideal’ dressing for a surgical incision and regional considerations in post-surgical incision care.
Results
Undisturbed wound healing
There was consensus across all regions regarding the importance of undisturbed wound healing (UWH) for surgical incisions.
There was recognition that UWH has been practised for many years, but only sporadically, and that it is now gaining attention, not only with respect to surgical incisions, but also for all other types of wounds. UWH was considered by the experts to have particular relevance for surgical incisions, due to the need to for protection of these wounds from contamination (as highlighted by WUWHS, 2016). Brindle and Farmer (2019) suggest benefits of UWH as including that:
- Healing is optimised if the wound remains undisturbed, in the absence of clinical reasons for doing so
- UWH reduces the risks of contamination and potential infection
- UWH yields savings in cost and healthcare professional time.
Experts in all regions concurred with these benefits of UWH, although the Australian panel highlighted the need for further strengthening of the evidence base to support the benefits of UWH (Sandy-Hodgetts et al, 2024a). The New Zealand panel highlighted the environmental impacts of frequent dressing changes, noting that UWH can yield benefits regarding more environmentally sustainable practices and better resource use (Sandy-Hodgetts et al, 2024b).
Experts in all regions considered that dressings on surgical incisions should be left in place for as long as possible and only changed if clinical indications require otherwise. Clinical indications for changing dressings identified by the experts included:
- Saturation of the dressing with exudate
- Leakage from the dressing
- Excessive bleeding
- Suspected infection
- Wound edge deterioration or dehiscence
- Loss of adherence of the dressing
- Skin irritation or an allergic response to the dressing.
Despite this consensus, the experts identified that local and regional practice varied. Across the regions, protocols for dressing wear time ranged from 2-14 days, with others indicating that dressings should remain in place until discharge, until suture removal or be changed on an individualised patient-centred basis or only if clinically needed, with one local recommendation for using wound glue in healthy patients with clean wounds and leaving wounds uncovered (multinational panel; Sandy-Hodgetts et al, 2022a).
An important contributor to this was identified by the experts as being “ritualistic practice”, with dressings often being changed at set times due to established local custom and practice, rather than because of clinical need. This practice was agreed by all experts to be suboptimal for the patient. Use of the right dressing, and education on the rationale for this, were agreed to be crucial to improve practice.
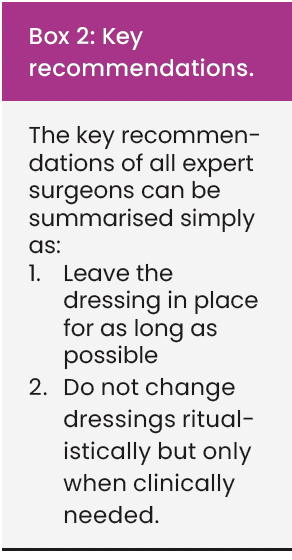
The key recommendations from the expert surgeons are summarised in Box 2.
Characteristics of an ‘ideal’ wound dressing for surgical incisions
The first consensus meeting (Morgan-Jones et al, 2019) identified the following as characteristics of an ‘ideal’ dressing for surgical incisions:
- Flexible and comfortable, so as not to impede the patient’s movement or cause damage to the skin
- Fixes well to the skin on application, even soon after skin disinfection
- Absorbent and able to manage exudate
- Skin protective (minimising the risk of blistering or irritation and not excessively adhesive)
- Waterproof, providing a good seal/barrier and allowing the patient to engage in personal hygiene activities
- Eliminates ‘dead space’ between the wound bed and dressing.
These characteristics were supported by experts in subsequent meetings, with additional characteristics also identified in some regions, with the Japanese panel identifying a wider range of considerations than all other panels (Yamada et al, 2025).
Experts in the APAC, Northern Europe, New Zealand and China regions highlighted considerations regarding patient comfort (including atraumatic removal), with the Africa panel noting the need to avoid provoking anxiety in patients (e.g. with a large dressing). It was noted that the dressing should be lightweight, soft, flexible and adaptive to the patient’s mobility after surgery. The Chinese panel additionally highlighted that use of a dressing that minimises discomfort can have a positive effect on patients’ engagement with their treatment, as well as improving quality of life and overall patient experience (Cao et al, 2025).
Ease of use (for both patients and health professionals) was identified as an additional consideration in most regions (Australia; Eastern Europe; India; Japan; Middle East; New Zealand; Northern Europe; China). The importance of anatomical location of the wound and need for dressings to be able to accommodate irregularly shaped and high-mobility areas (e.g. elbows and knees) was highlighted in several reports (Australia, Japan, Middle East and New Zealand).
The Middle Eastern, Japanese and Chinese panels in particular highlighted the importance of dressing properties that promote healing and prevention of infection, with the Japanese panel specifically highlighting antimicrobial properties (Yamada et al, 2025). The Chinese panel stressed the importance of dressings having antimicrobial or bacteriostatic properties to protect the incision during the vulnerable postoperative period, particularly for high-risk incisions, such as those involving implants, immunocompromised patients, or contaminated surgical sites (Cao et al, 2025).
Cost-effectiveness and affordability (for both patients and health systems) were identified as important in several regions (Australia, India, Japan, Middle East and New Zealand). The APAC, Australian and New Zealand panels highlighted that cost-effectiveness should address the whole treatment episode (including time, additional resources needed for the dressing change, number of dressing changes and total cost of healing the wound), not only the per-product cost of the dressing. The New Zealand panel also identified environmental sustainability and waste as important considerations (Sandy-Hodgetts et al, 2024b).
Regional variations
While there was a high degree of consensus across the regions, some region-specific issues were also identified.
Several reports (APAC, Indian, Chinese and multinational) indicated that considerations relating to the local climate, especially heat and humidity and geography, especially patients living in remote areas or needing to travel long distances for treatment influenced choice of dressing (e.g. waterproof) and when it was changed (e.g. prior to discharge).
Local customs and practices regarding bathing were highlighted by the Japanese panel. A further consideration raised only by the Japanese panel, and reflecting the country’s ageing population, was the need to consider presence of dementia when selecting a dressing. Obesity is a recognised risk for SWCs (ECDC, 2023) and was mentioned by some panels (e.g. Australia and Japan), with the Japanese panel suggesting that low levels of obesity in Japan contribute to the country’s low rate of SWCs.
The Chinese panel highlighted scar formation as a consideration. The “ideal” dressing can lessen tension on the incision, maintain skin smoothness, and lower the risk of keloid scar development, making it particularly suitable for patients who desire better cosmetic outcomes for their incisions following joint surgery (Cao et al, 2025).
Regional variation was present in the extent to which affordability was a consideration and there was also variation in whether this related to affordability for individual patients, as raised by the Indian panel or the healthcare setting (e.g. public versus private), as identified by the Australian and New Zealand panels. The APAC and multinational reports also noted that product availability varies across regions. A further regional variation, raised in reports from India and Japan, related to who has responsibility for selecting dressings and undertaking wound care.
Wider considerations
Most of the reports highlighted the importance of pre-operative preparation and consideration of individual patient circumstances, such as risk level, obesity, malnutrition and comorbidities and the nature of the surgical procedure (e.g. elective or emergency; simple or complex). The potential benefits of protocols such as Enhanced Recovery After Surgery, ERAS (https://erassociety.org/) were mentioned in several reports (APAC, multinational, Middle East, Northern Europe and China), although there was recognition that ERAS is not universally adopted.
The importance of consistent and standardised practice was identified in most reports, with the APAC and multinational reports highlighting the value of the World Health Organization’s WHO surgical checklist (https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery/tool-and-resources) in facilitating this.
A further consideration highlighted in several reports (APAC, India, multinational and Northern Europe) was the need for improved health professional education and training in the post-surgical incision care and recognition of SWCs. The Middle Eastern and New Zealand reports also highlighted the importance of patient education, with the latter highlighting the relevance of the country’s rurality in this.
Discussion
This article has brought together findings of 12 reports from consensus meetings held in a wide range of global regions between 2019 and 2025 and involving over 100 international surgeons and surgical experts. Although there were some local and regional variations, there was a high degree of consensus both within the panels and across regions regarding best practices for post-surgical incision care and dressing selection.
Experts identified the importance of protecting surgical incisions, minimising disturbance and supporting healing. There was strong consensus across all regions regarding the importance of UWH for surgical incisions, with experts advocating dressing changes for these wounds only when clinically necessary. There is some evidence in the research literature to support this recommendation (Brindle and Farmer, 2019) and it concurs with the views of other international wound care professionals (Davies et al, 2019); however, as the Australian panel noted, further research on UWH is needed.
Characteristics of an “ideal” dressing for surgical incisions for which there was consensus in all regions were that it is: flexible and comfortable; fixes well to the skin; absorbent; skin protective; waterproof and eliminates “dead space” between the wound bed and dressing, with additional characteristics, such as patient comfort, ease of use, promotion of healing, prevention of infection, cost-effectiveness and scar reduction also being identified in some regions. Regional differences and considerations (e.g. climate, geography and availability of resources), as well as wound location and individual patient needs were considered. This concurs with the WUWHS (2022) consensus report stating that safeguarding the incision site is essential, especially in reducing the risk of SSI and SWD. Equally important for enhancing patient well-being and outcomes is establishing an optimal wound healing environment.
Consistent care, education and standardisation of practice were highlighted as essential for improving patient outcomes globally and in promoting a much-needed move away from ‘ritualised practice’. Implementation and adoption of standardised perioperative approaches, including those proposed by the ERAS are designed to reduce surgical stress, improve recovery and enhance patient outcomes using a multidisciplinary approach throughout the pre, intra and post operative periods. However, it is recognised this can be challenging due to resistance to change, lack of resources and differing global approached to healthcare (Özçelik, 2024).
Summary
UWH is central to modern postoperative incision care. Healthcare providers can foster an optimal healing environment, minimise complications, and enhance patient outcomes by selecting the right dressings and following best practice. Effective incision management relies on continuous education, active patient involvement, and an awareness of regional considerations. Experts emphasised that dressing changes should be based on clinical need rather than routine practice, with wear times varying from 2 to 14 days across regions. Some protocols allowed dressings to remain in place until discharge or suture removal, while one regional approach favoured wound glue for healthy patients with clean wounds. See Box 3 for a summary of the concept of UWH as defined by the expert surgeons.
An ideal wound dressing should be flexible, well-adherent, absorbent, waterproof, and protective, eliminating dead space between the wound and dressing. Regional factors require consideration to include climate, geography, cultural customs, and demographics. With the ageing population, dementia-related considerations were highlighted alongside affordability.
Appendix 1: The Incision Care Expert Surgical Panel
Rhidian Morgan Jones (Chair), Orthopaedic Consultant and Major Revision Centre Lead, Colchester Hospital, East Suffolk & North Essex Foundation Trust, Essex, UK
Adesoji Ademuyiwa, Professor of Surgery (Paediatric and Surgical Epidemiology), University of Lagos; Honorary Consultant and Chief, Lagos University Teaching Hospital, Lagos, Nigeria
Mohamed Muath Adi, Consultant Orthopaedic Surgeon, Abu Dhabi, United Arab Emirates
Ali Al Belooshi, Consultant Orthopaedic Surgeon, Mediclinic, United Arab Emirates
Saed Al Habib, Consultant Plastic Surgeon, Saudi Arabia
Salem Al Nuiami, Consultant Orthopaedic Surgeon, Zayed Military Hospital, Abu Dhabi, United Arab Emirates
Jonas Andersen, Orthopaedic Consultant, Steno Diabetes Centre, Copenhagen, Denmark
Hideyuki Arima, Department of Orthopaedic Surgery, Hamamatsu University School of Medicine, Shizuoka, Japan
Peter Awang, Specialist General Surgeon, Bokamoso Private Hospital, Gaborone, Botswana
Hasan Aziz, Plastic Surgeon, Kuwait
Georges Balenda, General Surgeon, Louis Pasteur Hospital Medical Centre, Pretoria, South Africa
Prof Tomasz Banasiewicz, Head of Department of General Endocrine Surgery and Gastrointestinal Oncology, Poznań University of Medical Sciences, Poznań, Poland
Sameek Bhattacharya, Plastic Surgeon, Head of Burns and Plastic Surgery, ABVIMS & Ram Manohar Lohia Hospital, New Delhi, India
Michael Bishay, Consultant Orthopaedic Surgeon, Royal United Hospital, Bath, UK
Pål Borgen, Orthopaedic Surgeon, Martina Hansens Hospital, Sandvik, Norway
Dr Alessandra Canal, Plastic and Reconstructive Surgery, Auckland, New Zealand
Li Cao, Orthopaedic Surgeon, First Affiliated Hospital of Xinjiang Medical University, China
Dr Belinda Chan, General Surgeon, Strathfield, Australia
Hua Chen, PLA General Hospital, China
Dr S Vetrivel Chezhian, Professor of Orthopaedics, Coimbatore Medical College, Coimbatore, India
Hyonmin Choe, Department of Orthopaedic Surgery, Yokohama City University, Kanagawa, Japan
Timo Clasen, Consultant in Visceral Surgery and Wound Care Specialist, Agaplesion Deiakonieklinikum in Rotenburg/Wuemme, Germany
Dr Mark Cullinan, General Surgeon, Melbourne, Australia
Cai Daozhang, Doctor of Sport Medicine, Third Affiliated Hospital of Southern Medical University, China
Dr Ján Debre, Head Orthopaedic Surgeon, Šumperk Hospital, Šumperk, Czech Republic
Dr Radek Dolezel, General and Oncology Surgeon, Charles University and Military University Hospital, Prague, Czech Republic
Tomomi Fukuhara, Traumatology and Reconstructive Surgery Center, Saiseikai Niigata Kenoh Kikan Hospital, Niigata, Japan
Dr Tibor Gunther, Chief Surgeon, Trauma and Orthopaedic Department, Petz Aladar University Hospital, Gyor, Hungary
José A Hernández-Hermoso, Chairman of Orthopaedic Surgery and Traumatology, Germans Trias; Pujol University Hospital, Barcelona, Spain; Associate Professor UAB
Professor Andrew Hill, General Surgery, Auckland, New Zealand
Kushal Hippalgaonkar, Orthopaedic Surgeon; Executive Director, Sunshine Bone and Joint Institute, KIMS-Sunshine Hospitals, Hyderabad, India
Naoyuki Hirasawa, Department of Orthopaedic Surgery, Hokusuikai Kinen Hospital, Ibaraki, Japan
Jinghui Huang, Xijing Hospital of Air Force Medical University, China
Lee Sung Hyun, Orthopaedic Surgeon, Wonkwang University, Iksan Hospital, Korea
Nils Irsigler, Plastic and Reconstructive Surgeon, Zuid-Afrikaans Hospital, Pretoria, South Africa
Baochao Ji, The First Affiliated Hospital of Xinjiang Medical University, China
Dr Wei Jianxia, Obstetrician and Gynaecologist, Department of Obstetrics, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing, China
Professor Song Min Jong, Professor, College of Medicine, Catholic University of Korea, Seoul, Korea
Dr Wang Junjie, Senior Consultant, Obstetrician and Gynaecologist, KK Women’s and Children’s Hospital, Singapore
Ahmed Khazbak, Plastic Surgeon, Ministry of Health and Prevention, United Arab Emirates
Tay Boon Keng, Orthopaedic Surgeon, Singapore General Hospital, Singapore
Junjiro Kobayashi, Cardiovascular Surgeon, National Cerebral and Cardiovascular Center, Osaka, Japan
Asuri Krishna, Additional Professor, Professor of Surgery, All India Institute of Medical Sciences Delhi, New Delhi, India
Colin M Krüger, Chief Oncologic Surgeon and Robotic Surgery Specialist, Ruedersdorf b. Berlin, Germany
Gigy Raj Kulangara, Head of Department and Senior Consultant, Plastic, Reconstructive and Microvascular Surgery, Rajagiri Hospital, India
John C Lantis, Vice Chairman of the Department of Surgery, Chief of Vascular and Endovascular Surgery, Director of Surgical Clinical Research, Professor of Surgery at the Icahn School of Medicine, Mount Sinai West, New York, New York, USA
Associate Professor Edmund Leung, Faculty of Medical Science, University of Auckland; International Ambassador, British Association of Surgical Oncology, Royal College of Surgeons of England; Honorary Senior Lecturer, School of Medicine, Cardiff University, UK
Huiwu Li, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, China
Yang Li, Peking University Third Hospital, China
Tao Liu, Henan Provincial People’s Hospital, China
Christiaan Andre Loubser, Consultant, Busamed Bram Fischer International Airport Hospital, Bloemfontein, South Africa
Songcen Lyu, The Second Affiliated Hospital of Harbin Medical University, China
Niveshni Maistry, Paediatric Surgical Registrar, Nelson Mandela’s Children’s Hospital, Johannesburg, South Africa
Xinzhan Mao, The Second Xiangya Hospital of Central South University, China
Aditya Menon, Orthopaedic Surgeon, PD Hinduja Hospital and Medical Research Centre, Mumbai, India
Riju R Menon, Clinical Professor, Department of General Surgery, Amrita Institute of Medical Sciences Hospital, Kochi, India
Yoko Miura, Joint Reconstruction Center, Funabashi Orthopaedic Hospital, Chiba, Japan
Masaki Mizushima, Department of Orthopaedic Surgery, Yonemori Hospital, Kagoshima, Japan
James Murray, AOC, Southmead Hospital, University of Bristol and Knee Specialists Bristol, UK
Bhushan Nariani, Orthopaedic Surgeon, BL Kapur Super Speciality Hospital, India
Liezl Naude, Clinical Nurse Specialist and Founder, Eloquent Learning Health, Pretoria, South Africa
Dr Chia Yin Nin, Senior Consultant, Obstetrician and Gynaecologist, Gynaecology & Oncology Specialists, Gleneagles Hospital, Singapore
Neford Oendo Ongaro, Orthopaedic Surgeon, NEFRIS, Eldoret, Kenya
Jorma Pajamaki, Senior Orthopaedic Specialist, Pihlajalinna Group, Finland
Associate Professor Krasean Panyakhamlerd, Department of Obstetrics and Gynaecology, Faculty of Medicine, Chulalongkorn University Bangkok, Thailand
Dr Örs Pécsi, Trauma and Orthopaedic Surgeon, Erzsébet Kórház, Budapest, Hungary
Antonio Pellegrini, Consultant Orthopaedic Surgeon, IRCCS Istituto Ortopedico Galeazzi, Centre for Reconstructive Surgery and Osteoarticular Infection, Milan, Italy
Ashish Phadnis, Orthopaedic Surgeon, Department of Orthopaedics, Jupiter Hospital, Thane, India
Dr Fransiscus OH Prasetyadi, Obstetrician and Gynaecologist, Dr Ramelan Naval Central Hospital, Surabaya, Indonesia
Dr Dinakar Rai, Head of Department of Orthopaedics, PSG Institute of Medical Sciences, Coimbatore, India
Assistant Professor Dr Kylie Sandy-Hodgetts, ISWCAP President, Australia
Sujata Sarabahi, Head of Burns and Plastic Surgery, VMMC and Safdarjung Hospital, New Delhi, India
Dr C Savitha, Medical Superintendent and Professor, Department of OBG, Bangalore Medical College and Research Institute, India
Dr Ben Schwarz, Orthopaedic Surgeon, Sydney, Australia
Prof Dr Rajasekaran Shanmuganathan, Chairman, Department of Orthopaedics, Trauma and Spine Surgery, Ganga Hospital, Coimbatore, India
Dr Marianna Sioson, Consultant Director, Perioperative Medicine-ERAS, The Medical City Ortigas, Manila, Philippines
Dr Michael Solomon, Orthopaedic Surgeon, Randwick, Australia
Dr Tokumasa Suemitsu, Department of Obstetrics and Gynaecology, The Jikei University School of Medicine, Tokyo, Japan
Li Sun, Guizhou Provincial People’s Hospital, China
Dr Antoni Szczepanik, General and Oncology Surgeon, Department of General, Oncological, Gastroenterological and Transplant Surgery, Jagiellonian University Medical College, Krakow, Poland
Shunsuke Takahara, Department of Orthopaedic Surgery, Hyogo Prefectural Kakogawa Medical Center, Hyogo, Japan
Dr Eric Tan, MBChB, MRCS, CCBST, FRCS (Plast), Plastic Surgery, Hamilton, New Zealand
Dr Steven Tan, Obstetrician and Gynaecologist, St Leonards, Australia
Samih Tarabichi, Consultant Orthopaedic Surgeon and Chairman, Tarabichi Centre of Joint Surgery, Alzahra Hospital, Dubai
Gulnaz Tariq, United Arab Emirates
Mazen Tayeb, Arthroplasty Hip and Knee Surgeon at Security Forces Hospital, Saudi Arabia
Hua Tian, Peking University Third Hospital, China
Haruki Ueda, Department of Orthopaedic Surgery, Nasu Red Cross Hospital, Tochigi, Japan
Takenori Uehara, Department of Orthopaedic Surgery, NHO Okayama Medical Center, Okayama, Japan
Dr Michael Van Der Griend, Obstetrician and Gynaecologist, St Leonards, Australia
Zhavandre Van der Merwe, Advanced Wound Care Specialist, 4 Wounds Wound Care Practice, Pretoria, South Africa
Kate van Harselaar, Gynaecology, Fertility Specialist, Obstetrician; Clinical Director, Dunedin New Zealand
Weijun Wang, Nanjing Drum Tower Hospital, China
Weishan Wang, The First Affiliated Hospital of Shihezi University School of Medicine, China
Prof Maciej Wilczak, Director, Department of Mother’s and Child’s Health, Gynecology and Obstetrics University Hospital, Poznań University of Medical Sciences, Poznań, Poland
Christian Willy, Professor of Surgery and Head of Department, Trauma & Orthopaedic Surgery, Septic & Reconstructive Surgery, Research and Treatment Centre for Complex Combat Injuries, Wound Centre (ICW e.V.), Military Hospital Berlin, Germany
Koji Yamada, Director, Nakanoshima Orthopaedics, Kanagawa, Japan
Yukichi Zenke, Trauma Reconstruction Center, University of Occupational and Environmental Health, Fukuoka, Japan
Jingwei Zhang, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, China
Haiyan Zhao, The First Hospital of Lanzhou University, China
