Journey from the Step-by-Step Diabetic Foot programme to Train the Foot Healthcare Professionals: 22 years of preventing amputation globally
Received:
Accepted:
Published:
Authors: Zulfiqarali G Abbas, Harikrishna KR Nair,
Citation:
Abbas ZG, Nair HKR (2025) Journey from the Step-by-Step Diabetic Foot programme to Train the Foot Healthcare Professionals: 22 years of preventing amputation globally. Global Wound Care Journal 1(1): 42-49
Ethical approval
This study did not require ethical approval as no patient-identifiable information was included.
Conflicts of interest
Zulfiqarali G Abbas is a member of the editorial board and Harikrishna KR Nair is the editor-in-chief of the Global Wound Care Journal
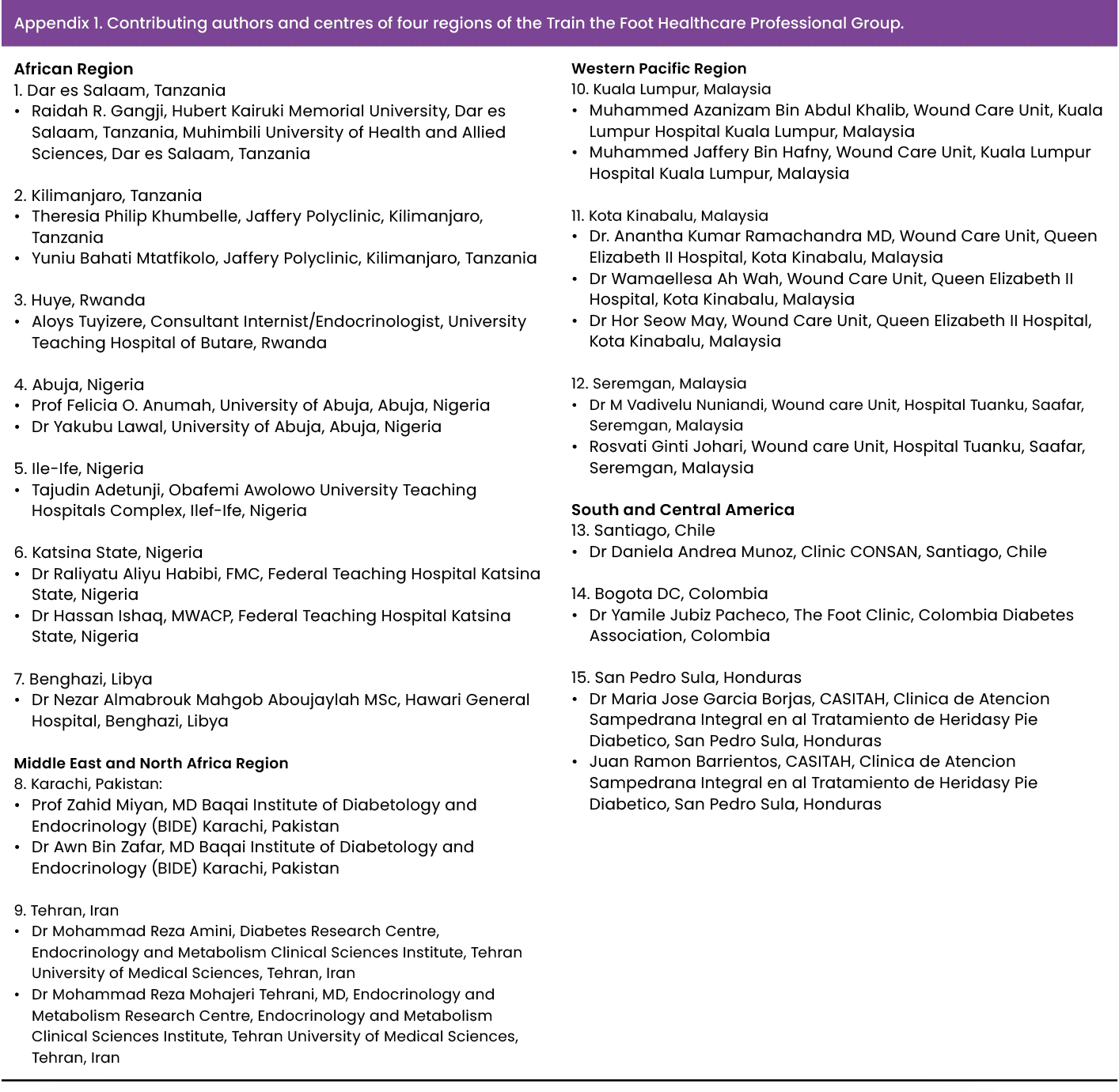
Acknowledgements: This work was made possible through initial funding from the World Diabetes Foundation and academic support from the International Diabetes Federation, the International Working Group on the Diabetic Foot, the Diabetic Foot Society of India, and the Muhimbili University College of Health Sciences, Dar es Salaam, Tanzania. The first pilot project core team of the SbS training program in Tanzania was initiated in 2003 by Zulfiqarali G Abbas (Tanzania), the late Sharad Pendsey (India), Vijay Viswanathan (India), Karel Bakker (the Netherlands) and the late Alethea Foster (UK). We thank the core team of the Train the Foot Trainer and Train the Foot Healthcare Professionals and executive board members of D-Foot International (2023-25). We also thank excellent secretariat assistance in Dar es Salaam, Tanzania.
Corresponding author:
Zulfiqarali G Abbas, Abbas Medical Centre, P. O. Box 21361, Dar es Salaam, Tanzania. Email: zgabbas@hotmail.com
DOI: https://doi.org/10.63896/gwcj.1.1.42
High rates of morbidity and mortality are associated with diabetes-related foot complications, which are on the rise worldwide. Between 40% and 60% of all lower extremity non-traumatic amputations performed globally are on patients with diabetes. Every 20 seconds, a lower limb is lost to diabetes worldwide, yet the majority of these amputations could have been prevented with simple foot care interventions, regular screening and proper education. Despite this urgent need, healthcare professionals remain insufficiently trained in delivering simple yet effective diabetic foot care, leaving patients vulnerable to avoidable amputations. Amputation rates can be decreased by up to 85% by prophylactic measures, close patient monitoring, multidisciplinary treatment of foot ulcers, and education of healthcare staff on proper foot care. The Step-by-Step (SbS) Diabetic Foot programme, which was piloted and implemented in Tanzania and India in 2003, is an example of education. Crucially, the research was linked to a decrease of more than 50% in amputation rates in Tanzania. Due to the success of the programme, there is a growing demand for the adoption of the SbS programme in other countries. D-Foot International launched the Train the Foot Healthcare Professionals programme to overcome the challenges of reaching every country. The goal was to bring trainers from various nations in the region together and train healthcare professionals to execute SbS programmes when they return to their home countries. This paper provides a concise description of this innovative and successful implementation effort. The 22-year journey began in Tanzania in 2003 and culminated in global healthcare professional training, serving as a working model to reduce amputation and mortality.
Africa (1.5 billion; 18%) and Asia (4.8 billion; 59%) account for 77% of the world’s population. Diabetes affects 80% of people in low- and middle-income countries (LMICs), while 20% live in high-income nations (Atun et al, 2017; Abbas and Bal, 2019; Abbas, 2020, 2021; Abbas and Boulton, 2022; International Diabetes Federation [IDF], 2025).
The International Diabetes Federation (2025) predicts that LMICs will have the biggest increases in diabetes prevalence and will bear a significant burden over the next 20 years. It is anticipated to become the most common health issue in emerging countries and will continue to be a prominent cause of morbidity and mortality in all countries (Abbas and Bal, 2019; Abbas, 2020; 2021; Abbas and Boulton, 2022). Diabetes-related foot complications (DRFCs) have the highest morbidity and mortality of all diabetes complications (Abbas and Bal, 2019; Abbas, 2021, 2020; Abbas and Boulton, 2022).
Diabetes is one of the fastest-growing worldwide health problems in the 21st century. Diabetes affected approximately 588.7 million people in 2024, which is predicted to increase to 852.5 million by 2050. Furthermore, it is anticipated that 634.8 million people will have impaired glucose tolerance and will increase to 846.5 million by 2050 (IDF, 2025). With the increase in diabetes, each region of the world is at a distinct stage of epidemiological change (Abbas and Bal, 2019; Abbas, 2020, 2021; Abbas and Boulton, 2022; IDF, 2025). Urbanisation, lifestyle changes, the demographic shift towards an older population, and increased risk factors, such as obesity and physical inactivity, have all contributed to the rising prevalence of diabetes. Sub-Saharan Africa, the Middle East and North Africa, South and Central America, the Western Pacific, and Southeast Asia are all seeing rapid growth and increasing prosperity (Atun et al, 2017; Abbas and Bal, 2019; Abbas, 2020, 2021; Abbas and Boulton, 2022; IDF, 2025).
DRFCs have the greatest morbidity and mortality rates of any type of diabetes complication. It is estimated that more than 20 million people worldwide have DRFCs, which remains a prominent source of sickness and death (Abbas, 2020, 2021; Abbas and Boulton, 2022). Every year, an estimated 2 million people with DRFCs require an amputation, with many requiring hospitalisation due to infections or complications of peripheral artery disease (Abbas and Bal, 2019; Abbas, 2020, 2021).
Diabetes is thought to account for 40–60% of all lower limb non-traumatic amputations performed worldwide (Abbas and Bal, 2019; Abbas, 2020, 2021; Abbas and Boulton, 2022; Senneville et al, 2023; Schaper et al, 2024). The lifetime risk of developing DRFCs is estimated to be between 15% and 34%, whereas the annual incidence is between 2.5% and 5% worldwide (Singh et al, 2005; Armstrong et al, 2017). The consequences of DRFCs include substantial impairment, lower quality of life, a shorter life expectancy and high healthcare costs (Cavanagh et al, 2012; Atun et al, 2017; Abbas and Bal, 2019; Abbas, 2020, 2021; Abbas and Boulton, 2022; Senneville et al, 2023; Schaper et al, 2024; IDF, 2025).
It is predicted that diabetes cost the world economy approximately US$1.3 trillion in 2015 and the global burden will reach US$2.5 trillion by 2030 if historical patterns continue (Bommer et al, 2018; Dhatariya et al, 2025). DRFC management accounted for 30% of the US$237 billion in direct diabetes spending in 2017 (Armstrong et al, 2020; Dhatariya et al, 2025). Similarly, diabetic foot ulcers (DFU) are estimated to cost the UK National Health Service 0.9% of its total budget (Kerr et al, 2019; Dhatariya et al, 2025). Despite the high prevalence, there is a dearth of data on the financial cost of DRFCs in poor nations (Abbas, 2017; Khan et al, 2018; Abbas and Boulton, 2022; Dhatariya et al, 2025). DRFC management received about 6% of Barbados’ national health budget (Greenidge et al, 2022; Dhatariya et al, 2025). A Brazilian study emphasised the need for greater outpatient care to lessen the cost burden of DRFCs on both individuals and the healthcare system (Toscano et al, 2018; Greenidge et al, 2022). The authors concluded that US$333.5 million was spent on outpatient DRFC care, compared to US$27.7 million for inpatient care. However, these figures did not include all expenses because indirect costs were not taken into consideration.
A recent study examined the cost of DRFCs in seven regions from 51 centres: four from North America and the Caribbean, nine from Africa, 11 from Europe, nine from the Middle East and North Africa, four from South and Central America, six from Southeast Asia (all from India) and eight from the Western Pacific (Dhatariya et al, 2025).
The cost of treating two hypothetical cases of wounds 1 and 2 were sent to all the centres. The average estimated cost of treating wound 1 was $2,942, ranging from $79 in Vellore, India, to $17,758 in Greece, with the relative costs compared to those of North America and Caribbean ranging from 0.36 in South and Central America to 0.75 in Europe. The average time in months of salary required to cover the estimated costs of treating the wounds was 8.6 months, ranging from 0.3 months in Romania to 62.3 months in Egypt.
For the treatment of wound 2, the average estimated cost was projected to be $17,403, ranging from $546 in Sudan to $67,178 in the Dominican Republic, with the relative costs compared to those of North America and Caribbean ranging from 0.06 in Africa to 0.69 in South and Central America. The average time in months of salary needed to cover the estimated costs of treating the wound was 22.7 months, ranging from 0.2 months in Malaysia to 98.3 months in Chennai, India (Dhatariya et al, 2025).
Every 20 seconds, a leg is amputated owing to diabetes, despite the fact that the majority of them (around 85%) could have been averted with relatively modest measures backed by basic education on DRFCs (Abbas and Morbach, 2005; Bakker et al, 2006; Pendsey and Abbas, 2007; Abbas and Archibald, 2007a, 2007b; Abbas et al, 2011; Abbas, 2013; 2014; 2015; Baker et al, 2017; Schaper et al, 2024). DRFCs should be the responsibility of everybody who is involved in the care of patients with diabetes. However, in many parts of the world, healthcare professionals (HCPs) are not trained to deliver simple but effective diabetes-related foot care.
To bridge this gap, the “Step by Step” (SbS) Foot programme, was launched in 2003, aiming to educate HCPs in diabetic foot care. This initiative later expanded with Train the Foot Trainer and Train the Foot Healthcare Professional (TtFHCP) (Abbas and Morbach, 2005; Bakker et al, 2006; Pendsey and Abbas, 2007; Abbas and Archibald, 2007a, 2007b; Abbas et al, 2011; Abbas, 2013, 2014, 2015; Baker et al, 2017).
To assess the impact of these programmes, we conducted preventive educational studies to determine their effectiveness in improving patient outcomes. The objective of the current study was to evaluate the outcome of the SbS foot programme started in 2003, leading to TtFHCPs in 2025 in the preventive global rate of amputations and mortality.
The Step-by-Step Diabetic Foot programme for reducing amputation rates
Step-by-Step: background and perspective
It all started in March 2003, when nine members representing the sponsors visited Abbas Medical Centre in Dar es Salaam, Tanzania, and saw the huge problem of DRFCs. At the same time, it was decided and encouraged to set up an educational project for LMICs and to prepare a curriculum for training the trainer in DRFCs. Dr Karel Bakker, former chair of the International Working Group on the Diabetic Foot, International Consensus Guidelines and International Symposium of Diabetic Foot, said: “It was a turning point in the history of diabetic foot for the low- and middle-income countries.”
The SbS Diabetic Foot programme is organised and focused primarily on diabetes-related foot education, training, and support. It was developed and instituted through a collaboration with the International Working Group on the Diabetic Foot, the Diabetic Foot Society of India, the Muhimbili University College of Health Sciences Dar es Salaam, and the International Diabetes Federation Consultative Section (Abbas et al, 2011).
The goal was to assist doctors and nurses in the identification and characterisation of DRFCs and equip them to manage such complications effectively through a structured programme of education and training. Several meetings were held, and a pilot training programme was designed to improve diabetes-related foot care in LMICs (Abbas et al, 2011).
The aim of this programme was to improve diabetes-related foot care in the training of HCPs. The following objectives were set:
- To provide sustainable training for HCPs in the management of DRFCs
- To facilitate the cascade of information from HCPs who have undergone training to other HCPs and thus to export expertise
- To reduce the risk of DRFCs in people with diabetes
- To empower people with diabetes to care for their feet better, detect problems earlier and seek timely help when problems arise.
The novel aspect of this programme was that delegates had to attend as a team consisting of a doctor and nurse, thus promoting teamwork. The teaching, consisting of theory and practical sessions, was delivered by experienced national and international educators and/or clinicians. The first programmes started in the autumn of 2004 in Dar es Salaam, Tanzania (Abbas et al, 2011).
The SbS diabetes-related foot programme comprised two 3-day programmes set 1 year apart. The first programme covered the basics, and the second programme was more advanced. In the 12 months between attending the basic and advanced programmes, the delegates were asked to collect activity and outcome data (Abbas et al, 2011)
In addition, the SbS programme organisers developed a wide array of educational health material for HCPs who deal with diabetic foot in less-developed settings. These materials include written, visual and audiovisual information pertaining to diabetes and its complications, with particular emphasis on foot pathology and management, and are aimed at both patients and HCPs. The materials are issued to SbS programme participants at the time of registration for the seminars (Abbas et al, 2011).
In Tanzania, 15 teams were selected from 14 regions, with both the basic (2004) and advanced programmes (2005) being held in Dar es Salaam, chaired by Dr Zulfiqarali G Abbas. The results of these two pilot projects have been published elsewhere, but in summary, diabetic foot teams and centres were established with a significant increase in foot screening with an increase in foot ulcer referrals due to raised awareness (Abbas and Morbach, 2005; Bakker et al, 2006; Abbas and Archibald, 2007a, 2007b; Pendsey and Abbas, 2007; Abbas et al, 2011; Abbas, 2013, 2014, 2015). Additionally, 3 years after the training, the incidence of foot ulcers and amputations in Tanzania fell significantly with sustained diabetic foot services in all trained centres (Abbas et al, 2011).
Step-by-Step: outcomes
The SbS Diabetic Foot programme in Tanzania led to better management of patients with foot ulceration, resulting in an improved outcome among people with DFUs at local levels and fewer referrals to the secondary and tertiary referral care centre for amputation.
In Tanzania, the SbS Diabetic Foot programme has enabled functioning foot clinics independently or in combination with diabetes clinics across the country. The programme has also created awareness of DRFCs among patients, relatives of patients, and nursing and medical personnel involved in diabetes foot care. It has also highlighted the importance of the development and training of staff and employing additional and more skilled personnel (Abbas and Morbach, 2005; Bakker et al, 2006; Abbas and Archibald, 2007a, 2007b; Pendsey and Abbas, 2007; Abbas et al, 2011; Abbas, 2013, 2014, 2015).
To determine whether the SbS Diabetic Foot programme was effective in DFU patients’ outcomes, we monitored temporal trends in rates of major amputation among people with DFU in one of the centres that already had an established surveillance system for DFU. For this, we chose the diabetes clinic at Muhimbili National Hospital (MNH) in Dar es Salaam, Tanzania, where the principal investigator had been conducting active surveillance of upper and lower limb complications among diabetes patients since 1997.
From 2000 to 2008, a total of 4,234 patients with diabetes were admitted to MNH of whom 736 (17%) of those patients had an active foot ulcer. Ulcer occurrence in these patients peaked in 2005 and then declined over the subsequent years (Abbas and Archibald, 2007; Abbas, 2013, 2014). During the study period, the mean annual amputation rate was 17.6% for all DFU patients referred to MNH (Abbas et al, 2011).
Before the introduction of the SbS Diabetic Foot programme, amputation rates for MNH referrals were >1 standard deviation above the mean annual rate. After 2005, the amputation rates in patients referred to MNH decreased significantly and, by 2008, fell to almost two standard deviations below the mean (Abbas et al, 2011). A significant reduction in the number of amputations was noted at MNH after implementation of the SbS Diabetic foot programme, which may be due to early observation and management of DRFCs in trained centres in rural areas, compared with before training had been introduced and amputation rates were higher (Abbas et al, 2011).
For patients who are referred for foot care at MNH, the improved management at the primary care level is translated into better opportunities to save limbs in the tertiary care setting, leading to better outcomes (Abbas et al, 2011).
Step-by-Step foot projects from 2003 to 2012
The success of the SbS training programmes led to an increasing demand for the SbS programme to be expanded from Tanzania to other countries, including other African countries (Congo, Guinea, Botswana, Malawi, Zimbabwe, Ethiopia, Mali, Nigeria, Egypt, South Africa and Kenya) and outside Africa (India, Pakistan, Dubai, Mexico, Barbados, St Lucia, St Marteen, St Kitts, British Virgin Islands, Antigua, Grenada, Dominica, Trinidad and Tobago and and many other Caribbean islands).
Regional training
Inception of the Train the Foot Healthcare Professionals programme
The demand for the SbS programme to be implemented in other nations has grown as a result of the training programme’s success. It was not possible to visit every country to conduct the SbS programme. The idea emerged to bring together all the experts involved in DRFCs in each region, then they would return home and conduct the SbS programme.
Train the Foot Trainer was introduced to train diabetes-related foot experts in the country in each region to conduct SbS in their countries. Train the Foot Trainer was the initial programme after SbS, but later, in 2023, the TtFHCP programme was started by the executive committee of D-Foot International.
The idea was to bring trainers from different countries within a region together and train the HCPs who manage DRFCs to implement SbS programmes when they return to their home countries. Every HCP who works in diabetes clinics should be able to manage and disseminate the knowledge of DRFCs. The programme’s content was based on the SbS curriculum, with a particular emphasis on data collecting, fundraising, strategic planning, teaching and implementing the SbS programmes. A core team from the D-Foot International 2023–2025 term created this initiative. Over the course of 2–3 days, the TtHCPs curriculum consists of a number of formal lectures, interactive workshops, live case presentations, group discussions and demonstrations.
Aims of Train the Foot Healthcare Professionals programme
The aim of the TtFHCPs programme is train local HCPs in DRFCs within a global region to deliver effective, well-structured, sustainable training programmes with demonstrable outcomes. The objectives of the delegates of the TtFHCP are:
- To organise and implement an SbS training programme for their own country (educational, organisational and public relations) after attending a TtFHCP programme
- To identify barriers to implementation and find solutions for their needs
- To evaluate the delivered programme by collecting and disseminating outcomes of the programme on a national, regional and international scale
- To train the trainers from their own communities to deliver an SbS training programme
- To encourage, support and develop an ongoing mentorship programme for existing and new diabetes-related foot HCPs in their region
- To try to ensure that health ministers, health policymakers, patients and professional groups are involved and supportive
- To determine ways in which teams developed by the SbS can be sustained, supported and, where possible, incorporated into healthcare systems.
In order to attend the TtFHCP programme as a delegate, a selection process exists with certain eligibility criteria; this is to try to ensure that post-programme implementation is successful. This is vital as generally only two delegates can attend from each representing country, however, in some cases, more delegates can attend if a country is geographically large. The selection criteria include evidence of diabetes-related foot clinical activity, organisational skills, and collaboration and support from the patient organisation and the ministry of health. The team should comprise a physician, a surgeon and a nurse with a willingness to work collaboratively.
Delegates must be willing to organising committee stating the following:
They are prepared to implement a regional and national programme to prevent amputations related to diabetes, starting by upgrading their own centre of reference
They will formally report to the organising committee after 6, 12, 24 and 30 months
They will contribute to an anonymised data collection system in line with the international principles of data privacy and security.
The TtFHCP core team recognised from the outset there was a fundamental need for a standardised and useful dataset and collection method for all participating delegates and countries. The original intention of this was to help individuals, centres and countries collect activity and outcome data, thereby helping them to develop their practice and lobby for continuing support.
Equally, the team needed to be able to identify the impact of the programme and use this for further fundraising, programme refinement and future developments. It was also hoped that there would be the potential to compare activity and outcome data from different regions. The programme is intended to develop local, regional and national networks and study/working groups with sustainability of service and education development and referral pathways. It is hoped that the delegates will be instrumental in driving and implementing policy decision-making in their respective regions.
Finally, another key outcome is intended to be the provision of a support mechanism for local HCPs, encouraging the development of further national training programmes with a national faculty to meet local needs.
Train the Foot Trainer programme from 2012 to 2020
- South and Central America (14 countries): Brazil, Argentina, Bolivia, Chile, Cuba, Colombia, Mexico, Panama, Paraguay, Peru, Uruguay, Ecuador, Venezuela and Dominican Republic.
- Caribbean Islands (20 countries): Barbados, St Lucia, St Marteen, St Kitts, St Thomas, British Virgin Islands, Bermuda, Haiti, Jamaica, Belize, Curacao, Antigua, Grenada, Dominica, Tobago, Nevis, Barbuda, Guatemala, Cayman Islands and Trinidad.
- European region (18 countries): Albania, Armenia, Bosnia, Herzegovina, Bulgaria, Croatia, Estonia, Greece, Kosovo, Latvia, Lithuania, Poland, Romania, Serbia, Slovenia, Sweden, Turkey and Ukraine.
- Western Pacific (13 countries): Australia, China, Japan, South Korea, Singapore, Malaysia, Cambodia, Indonesia, the Philippines, Taiwan, Thailand, Vietnam and Mongolia.
- French-speaking countries (12 countries): Benin, Burkina Faso, Burundi, Cameroon, Democratic Republic of Congo, Côte d’Ivoire, Guinea, Rwanda, Senegal, Morocco, Algeria and Tunisia.
- Middle East and North Africa (14 countries): Algeria, Egypt, Iraq, Jordan, Lebanon, Libya, Morocco, Oman, Qatar, Saudi Arabia, Sudan, Syria, Tunisia and UAE.
Train the Foot Healthcare Professionals programme from 2023 to 2025
TtFHCP was conducted in six World Health Organization (WHO) regions, namely Sub-Saharan Africa, Europe, Middle East and North Africa, South and Central America, South East Asia and the Western Pacific. We will evaluate the cascading effect of education in prevention of ulcer leading to amputation and mortality.
- Southeast Asia (four countries): India, Bangladesh, Nepal and Sri Lanka.
- South and Central America (eight countries): Argentina, Brazil, Chile, Colombia, Honduras, Ecuador, Panama and Peru.
- Western Pacific (12 countries): Malaysia, Myanmar, Taiwan, Thailand, Vietnam, Mongolia, Australia, Cambodia, Indonesia, Philippines, South Korea and Singapore.
- European region (10 countries): Bosnia, North Macedonia, Slovenia, Croatia, Serbia, Romania, Kosovo, Czech Republic, Montenegro and Poland.
- Africa (11 countries): Tanzania, Kenya, Uganda, Rwanda, Ethiopia, Nigeria, Ghana, Zambia, Zimbabwe, Libya and Tunisia.
- Middle East and North Africa (five countries): Pakistan, Iran, Lebanon, Syria and Sudan.
Outcomes of Train the Foot Healthcare Professionals programme
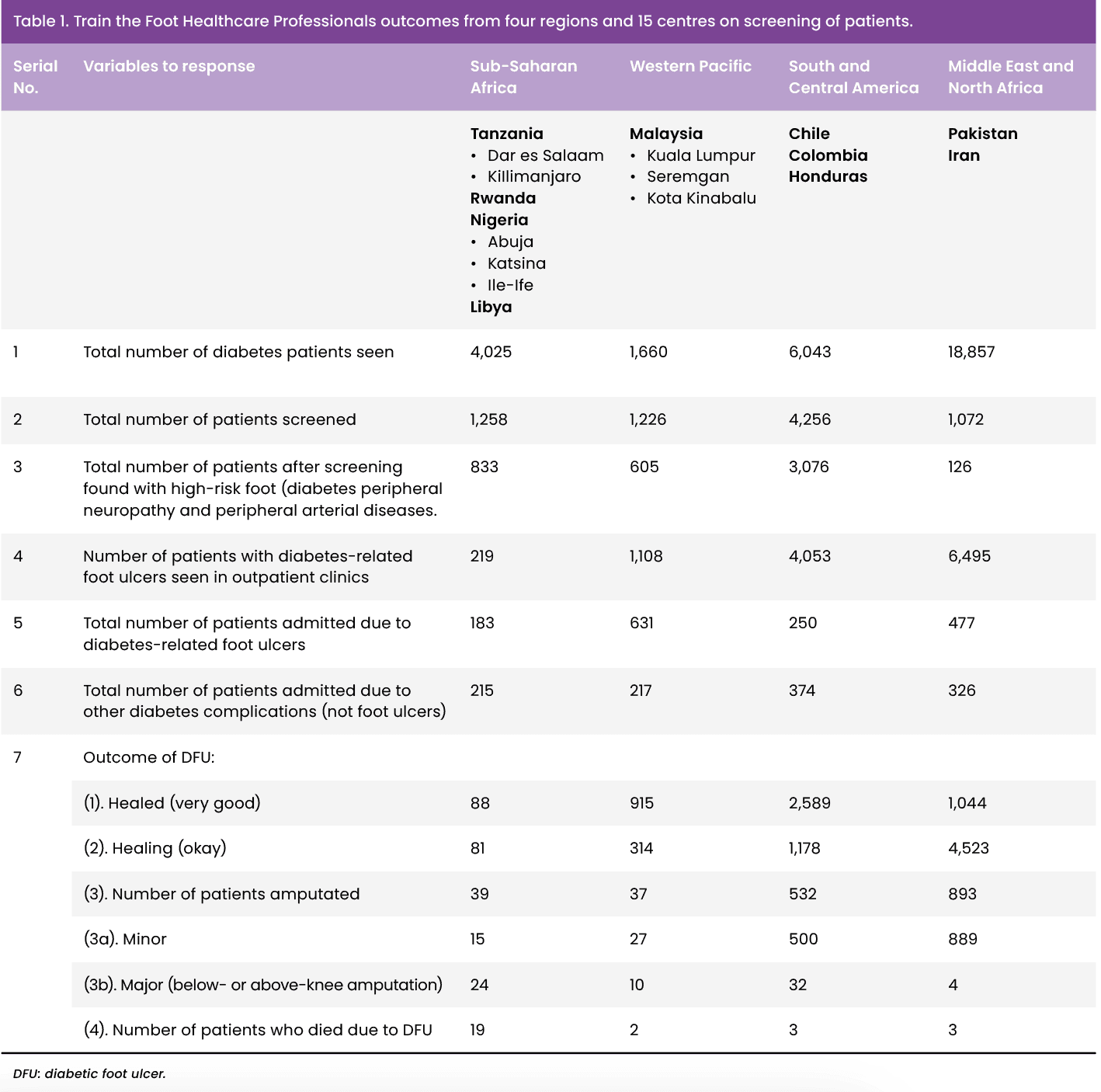
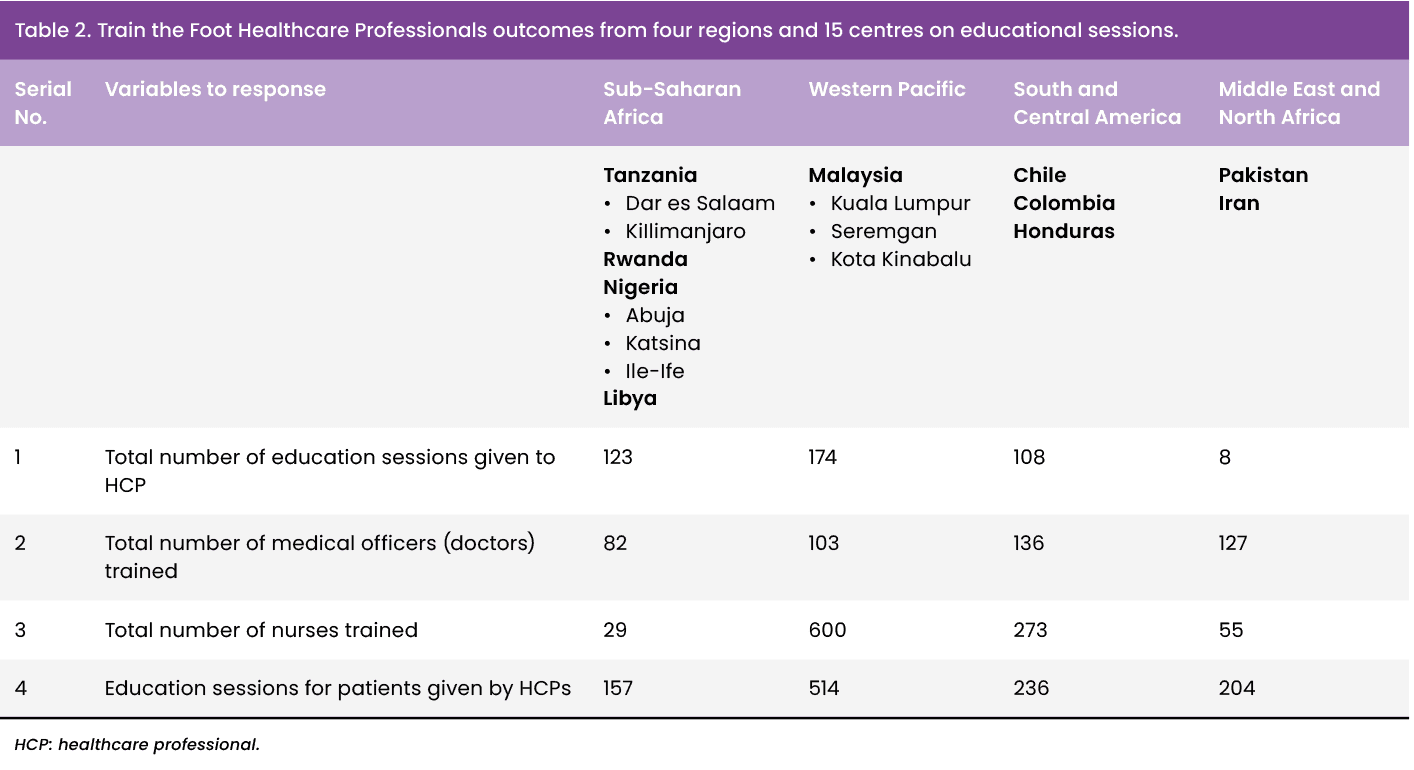
This article does not include a detailed outcome over the years from the TtFHCP programme that has taken place, as this will be reported elsewhere in the near future. Table 1 shows outcomes from four regions, including 15 countries altogether, regarding screening of the patients after training and Table 2 shows the educational sessions taken after TtFHCPs.
The future
The work has so far managed to cover six regions (Sub-Saharan Africa, South and Central America, Western Pacific, South East Asia, Middle East and North Africa, and Europe) of the seven world regions, and there is a desire to cover more. In addition, further implementation programmes and training modalities are being developed together with a supportive networking structure for all participants.
Conclusion
SbS Diabetic Foot programme is a unique educational programme started in low-income countries in 2003 in Dar es Salaam, Tanzania, and spread to middle-income countries and later higher-income countries. It has already covered 128 countries globally — 22 years of a journey of preventing amputation globally.
While it may not be possible to completely prevent foot ulcers, early intervention can effectively stop minor foot ulcers from progressing to serious complications, including infection, sepsis, osteomyelitis or gangrene. Education remains the most effective preventative strategy and should stand as a fundamental component of all diabetic foot care preventative programmes. It should be straightforward, repeated and aimed at both patients and HCPs.
Patients with diabetes need to be taught the value of taking good care of their feet and the necessity of seeing a doctor as soon as possible if they experience any foot-related symptoms. Ultimately, the ability of HCPs to instil the self-help and motivation necessary for people with diabetes wellbeing will determine success.
References:
