Nurses’ knowledge on pressure injury prevention in an acute hospital in Malta: a comparative cross-sectional study
Received:
Accepted:
Published:
Authors: Corinne Scicluna Ward, Anthony Xerri
Citation:
Scicluna Ward C, Xerri A (2025) Nurses’ knowledge on pressure injury prevention in an acute hospital in Malta: a comparative cross-sectional study. Global Wound Care Journal 1(1): 12–2
Ethical approval and consent to participate:
This study did not require ethical approval as no patient-identifiable information was included.
Consent for publication: Not applicable.
Conflicts of interest:
Corinne Scicluna Ward is a member of the Global Wound Care Journal editorial board
Corresponding author:
Corinne Scicluna Ward, Email: corinne.scicluna@um.edu.mt
DOI: https://doi.org/10.63896/gwcj.1.1.12
Background: Pressure injury (PI) prevention is an increasing concern for hospitals worldwide. Inadequate knowledge among nurses can contribute to improper PI prevention and management, potentially leading to complications, such as infections, delayed healing and increased patient discomfort. These complications may result in longer hospital stays and higher readmission rates, ultimately escalating healthcare costs. However, published local research on PI prevention in acute care settings remains limited, highlighting the need for further studies. Objectives: To investigate whether nurses working in an acute hospital in Malta are knowledgeable enough on PI prevention. To assess the barriers perceived by nurses that hinder them from applying the evidence-based PI prevention methods. To ascertain whether sociodemographic characteristics influence the nurses’ knowledge. Designs and Methods: A comparative, cross-sectional study was completed using a paper-based questionnaire to collect data. Copies were distributed among 626 nurses and obtained a response rate of 38.7% (n=242). Data collection tools included a Pressure Ulcer Knowledge Test and a survey assessing perceived barriers to the application of pressure injury prevention. Population: All nurses working in an acute hospital in Malta excluding nurses working in paediatrics, outpatients and emergency departments were invited to participate in the study. Results: A low level of knowledge (44.6%) regarding PI prevention was found. The number of perceived barriers hindering nurses from implementing PI prevention methods was also high (56.6%). Nurses with more clinical experience and who read relevant literature had a higher level of knowledge than other participants. Nurses with a degree perceived a larger number of barriers than nurses with a diploma, and statistical differences were found between the number of perceived barriers and clinical experience. Participants who read the literature or attended training perceived fewer barriers hindering them from applying appropriate PI prevention methods. A weak negative correlation was identified between nurses’ level of knowledge and the number of perceived barriers encountered by participants. Conclusion: Nurses in an acute Maltese hospital showed low knowledge and high perceived barriers to PI prevention. Experience, education and reading relevant literature improved outcomes. Targeted training and better access to resources are needed to enhance evidence-based practice and improve patient care.
Pressure Injuries (PI) can have a significant impact on the health, wellbeing and quality of life of patients in any type of hospital setting (Padula and Delarmente, 2019). They can cause pain and financial burdens, and nurses in acute hospitals play a crucial role in preventing and identifying these injuries. However, insufficient knowledge of PIs may negatively affect the care provided to patients (Mitchell, 2018). Often, these injuries go unnoticed until they are in advanced stages and, in such cases, preventive measures are only implemented after the injury has already developed. That is why the level of nurses’ knowledge on the topic of in any given hospital makes a difference.
Background
There are different terms used to refer to pressure injuries, such as pressure ulcers (PUs) or bed sores. For the purpose of this paper, the nomenclature used by the authors will be kept. PIs are best described as localised wounds to the skin and underlying layers and tissue, that are most commonly found over a bony prominence due to continuous pressure on the area (The European Pressure Ulcer Advisory Panel et al, 2019). Heels, elbows, ankles and the sacrum are the most common areas where PIs are formed and older people are more susceptible to developing them (Sugathapala et al, 2023). Additionally, patients who are bed-bound or have very minimal ability to move are the most prone to PIs (Sugathapala et al, 2023) and their development may significantly impact the general wellbeing of patients. Moreover, once established, they are challenging to treat and cause considerable distress to patients and their families (Su, 2021).
For a PI to occur, the peripheral pressure has to be greater than the arterial capillary pressure. Some of the most common markers of PI include discolouration, coolness or increased warmth non-blanching, pain or itching, and most commonly redness over the area. When tissue degradation occurs, the body’s systems work together to heal and replace the damaged tissue. Debris is cleared, and proteins are secreted to attract immune system cells that aid in tissue repair (Sinno and Prakash, 2013).
Rationale for the study
Preventing PIs is a matter of patient safety, and nurses should possess comprehensive knowledge in the field and be able to perform effective practices (Malinga et al, 2020). In addition, the literature indicates that an increase in training programmes, promoting continuous educational development, and updated guidelines can work towards decreasing the prevalence of PIs (Yan et al (2022). The suggestions made by the researchers, once implemented, would enhance nurses’ skills and knowledge (Gedamu et al, 2021). Nurses who attended training and read related articles demonstrated a notable improvement in their knowledge scores. Furthermore, conducting observational studies in future could help determine the actual practice of PI prevention rather than solely relying on perceived barriers (Ebi et al, 2019).
PI prevention directly exposes the quality of nursing patient care in a healthcare setting (Jiang et al, 2020). It is the role of nurses to prevent and assess the risk of PIs (Emami Zeydi et al, 2022).
Studies about Maltese nurses’ knowledge in wound care are minimal and so this led local researchers to delve into global studies. National studies can vary from global studies because every country has its own culture and this can influence nurses’ attitudes towards and knowledge on this particular subject. Thus, this study is important as it identified gaps in knowledge and recommended improvements regarding this subject that was culturally sensitive.
Aims, objectives and research questions
This study aimed to assess the level of knowledge on pressure injury prevention in an acute hospital in Malta. One of the objectives of this study was to establish an answer to two main research questions: “Are nurses in an acute hospital knowledgeable on the development of PIs and their prevention?” and “What are the perceived barriers to PI prevention in an acute hospital?”
Methods
Study design and questionnaire
The most suitable methodology for this kind of research was a comparative, cross-sectional quantitative study. A paper-based survey was chosen for data collection based on the questionnaire developed by Ebi et al (2019). The primary objective of the questionnaire was to convert knowledge variables into quantifiable, standardised segments that accurately depicted the nurses’ viewpoints concerning their level of knowledge on PI prevention.
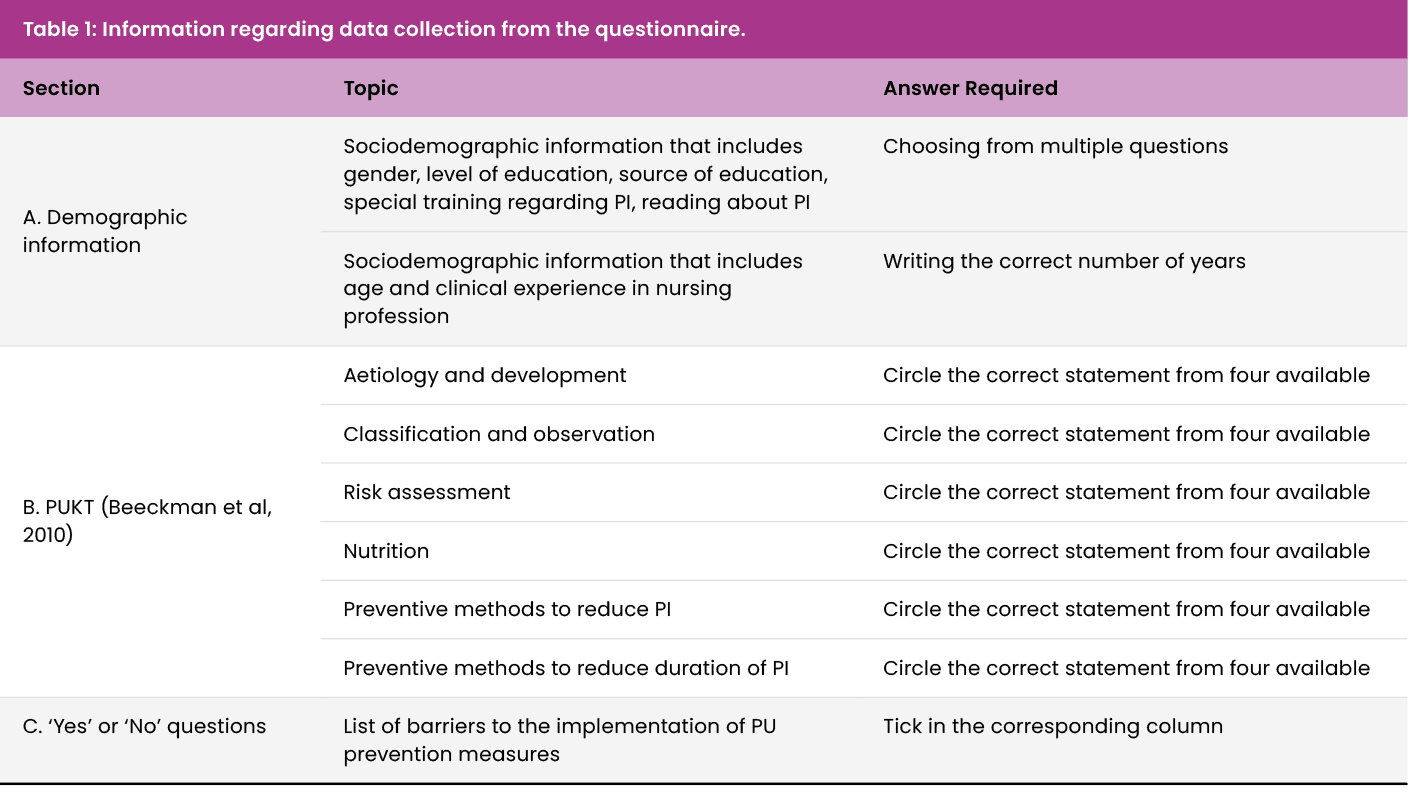
The questionnaire had three parts and an outline is presented in Table 1. The first part contained seven questions that addressed demographic data. The second part consisted of an English version of the Pressure Ulcer Knowledge Test (PUKT) tool (Beeckman et al, 2010). The third part comprised ‘Yes’ or ‘No’ questions on perceived barriers that might stop nurses from correctly implementing PI preventions. These three parts combined made up the final questionnaire that had already been tested and used in an existing study by Ebi et al (2019). Permission to use this questionnaire was obtained.
As a conceptual framework to guide this study, Benner’s nursing theory “From novice to expert” was used (Benner, 1982). According to this nursing theory, expert nurses acquire the skills and knowledge necessary to provide quality patient care through a combination of education and practical experience (Wayne, 2023).
Ethical considerations
Throughout this research, ethical standards were upheld at every phase to ensure the integrity and reliability of the results (Knottnerus et al, 2018). Prior to conducting the study, all necessary permissions were acquired. The study was then given the green light by the hospital’s Data Protection Officer and ethical approval was sought from the Faculty of Health Science’s University of Malta’s Research Ethics Committee. Following this, the necessary endorsement was successfully secured and consent from the intermediary of each ward was also obtained.
Results and discussion
The number of nurses eligible for this study was 626, and 242 questionnaires were completed and returned. This gave the study a 38.7% response rate with a 95% CI yielding a margin of error of 5%. The results showed that the mean level of knowledge score was 44.6%. This finding strongly indicates a low level of knowledge since the mean score obtained was less than half of the total achievable points.
Nurses’ overall level of knowledge regarding pressure injury prevention
Nurses who possess a sufficient level of knowledge are more effective in preventing PIs, and this can serve as a sign of the quality of nursing care (Wu et al, 2022). Indeed, the literature has consistently affirmed that having an insufficient level of knowledge regarding PI prevention can harm the effectiveness of preventative care measures (Dalvand et al, 2018). Research has shown that well-informed and well-trained nurses can successfully evaluate a patient’s risk of suffering PIs, implement preventive measures, and ensure rapid and suitable treatment when needed (Yann et al, 2022). Suitable training and education have been linked with a decrease in PU occurrence in healthcare settings (Awoke et al, 2022).
Table 2 presents the first six questions of the questionnaire, the instrument used for the data collection and these were related to the aetiology and development of PIs. In the first question, which was about what caused pressure injuries, only 11.6% got the correct answer, which is shown in the table. The majority of participants (88.4%) got the wrong answer. The second question in this section was related to whether thin patients were at an increased risk of developing a pressure injury, and more than half (58.7%) got the correct answer. The third question was related to what happened if the patient slid down while in a semi-upright position. Only 36.8% got the correct answer.
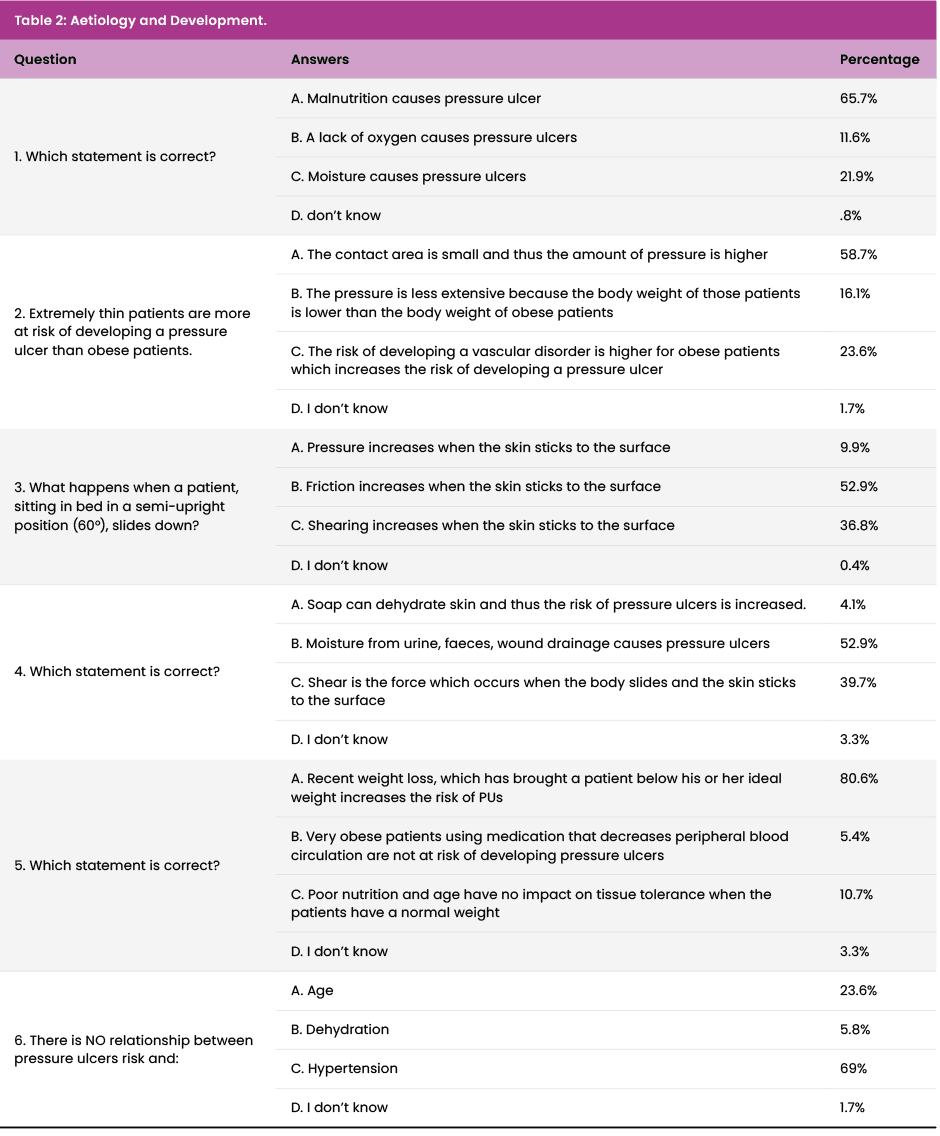
The majority of patients (52.9%) stated that it caused friction when the correct answer was ‘shearing’, suggesting that the majority of participants did not know the difference between friction and shearing. This was followed by another question related to what caused PIs and, again, only 39.7% got the correct answer, which was related to shearing. This was followed by a similar question on what caused PIs and 80.6% got the correct answer, which was related to the weight of the patient. This suggests that participants knew more about the influence of weight on the risk of PIs than on other factors, such as positioning. In the final question of this section, participants were asked which of the four options had no relationship with PIs. The correct answer was ‘hypertension’ (69%). The average knowledge score in this section was 49.4%.
Table 3 presents the second theme of the questionnaire, related to the classification and observation of PIs. The first question in this theme was related to stage 3 PIs and only 20.2% got the correct answer, while 79.8% got the answer wrong. The second question was about the stages of PIs as well, and 40.1% got the correct answer. The third question was related to friction and shear. In this section, 76% got the correct answer, quite a different result from that obtained in the first theme. The next question asked where pressure injuries were more likely to develop, and 66.5% stated the correct answer. This was followed by a question on how frequently the skin should be inspected and only 26.9% were correct. These findings suggest that although participants knew where and how PIs could develop, they did not have the knowledge to distinguish between stages and how often to inspect the skin. The average percentage score in this section was 31.5%.
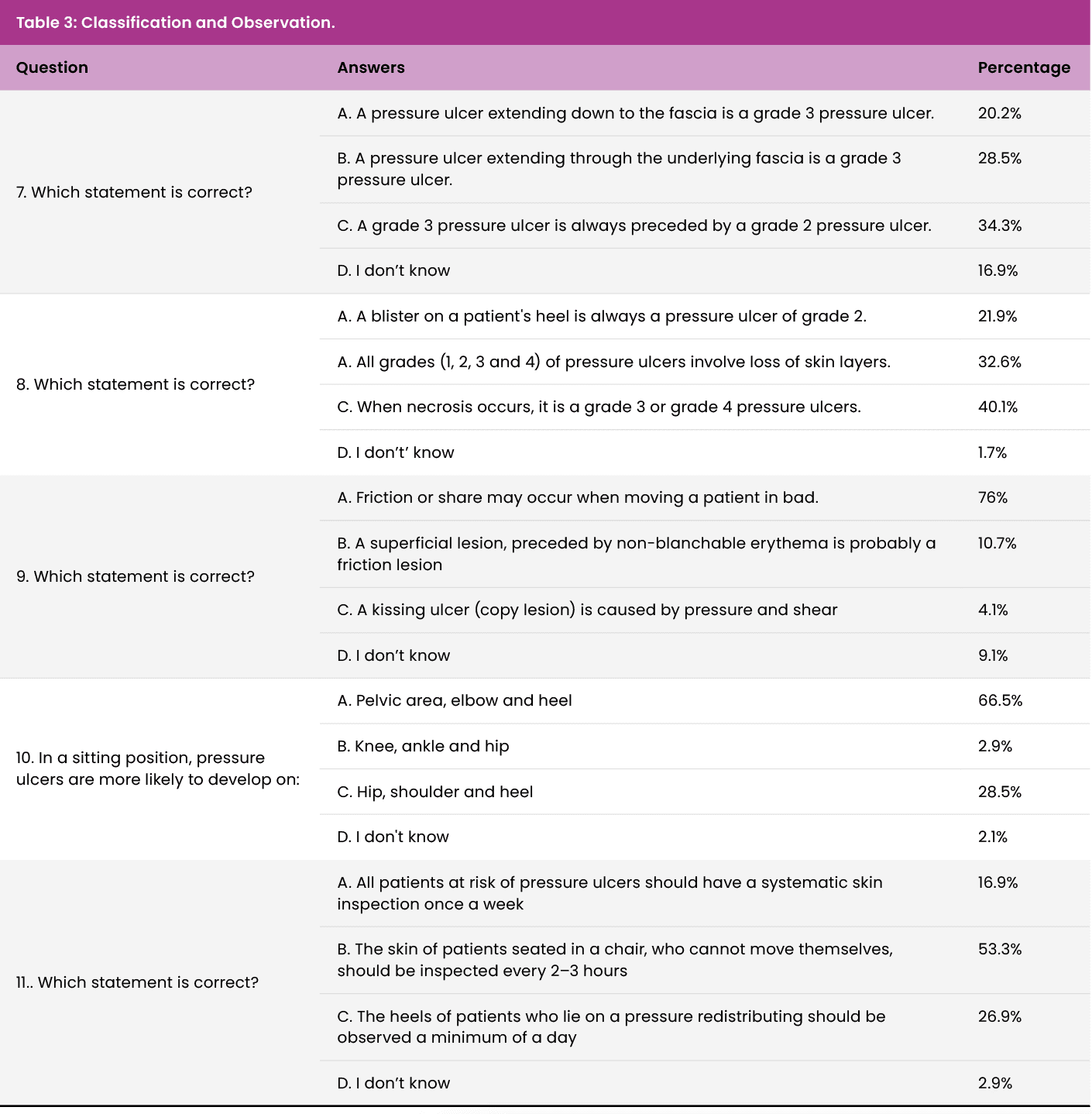
Table 4 presents the scores of the third theme of the questionnaire, related to risk assessment and nutrition. In the first question, related to risk assessment tools, only 36.4% answered correctly. This was followed by the second question on the risk of PIs and this was answered correctly by 34.3%. The third question in this theme was on nutrition concerning PIs and 35.5% had the correct answer. All the scores on this section were low, suggesting a poor level of knowledge on the subject of the theme. The average percentage level of knowledge in this section was 26.1%.
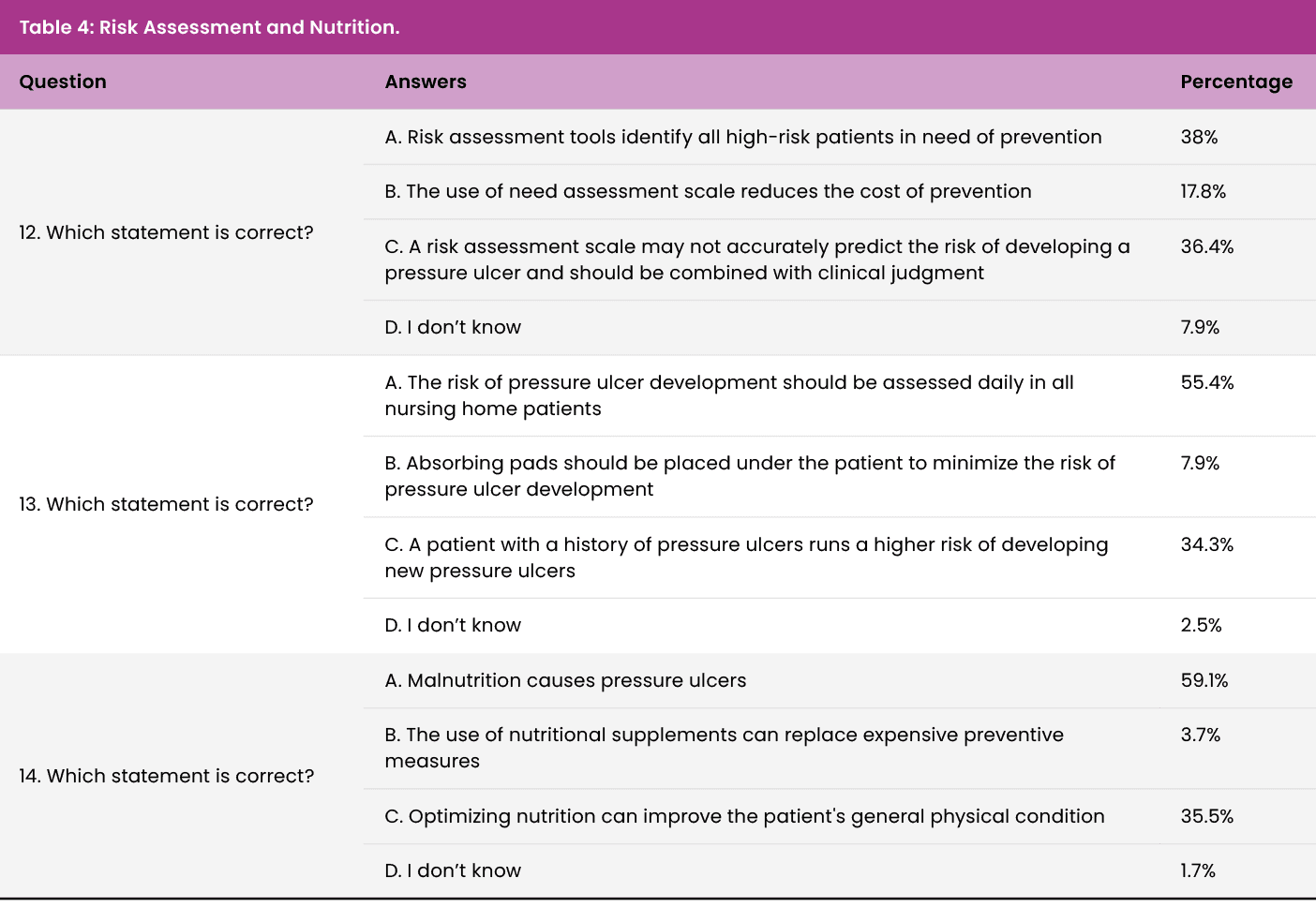
Table 5 presents the fourth theme of this questionnaire, on the preventive measures that reduce the amount of pressure and shear. This section consisted of seven questions. The first question was related to the positioning of the patient while in a sitting position. Only 21.1% gave the correct answer. The second and third questions in this section were also related to the repositioning techniques to reduce pressure injuries and again only 29.8% and 22.7%, respectively, answered correctly. The next question was on preventive devices applied when the patient is sitting down and 27.3% gave the correct answer. The last three questions were about different mattresses and 53.3%, 54.5% and 41.3%, respectively stated the correct answer. These findings suggest a poor level of knowledge on the preventive measures that reduce the occurrence of PIs. The average percentage level of knowledge in this section was 35.7%.
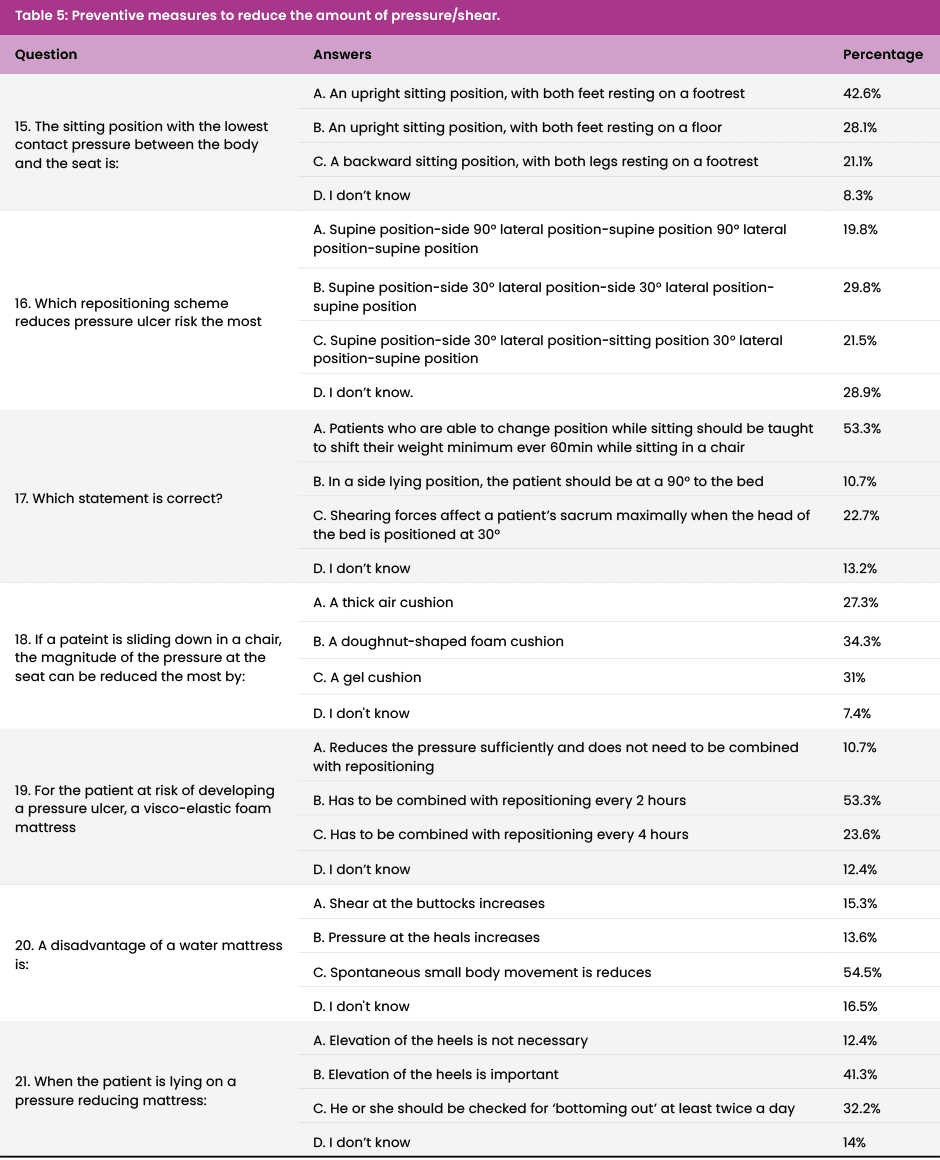
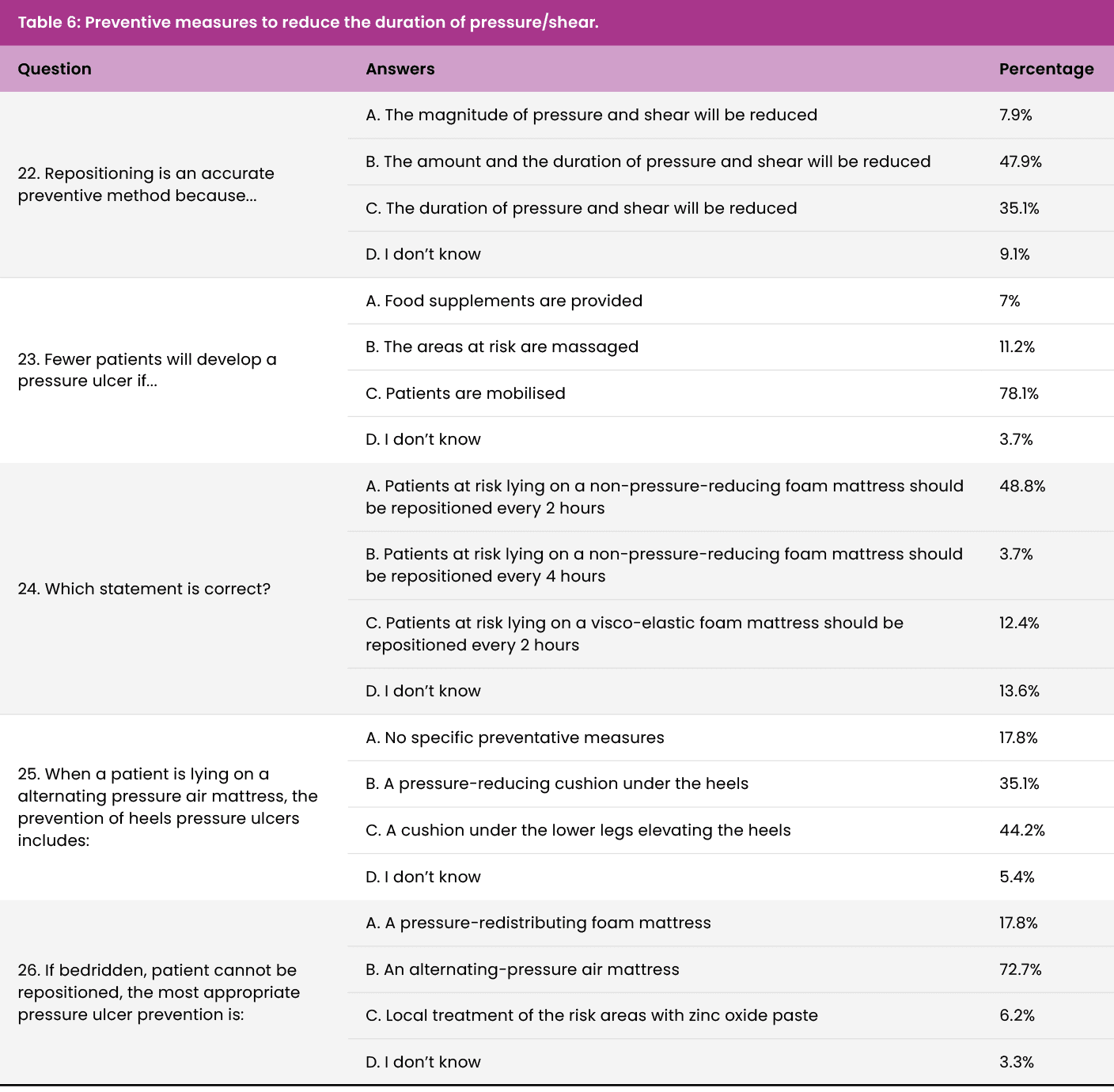
Table 6 presents the next theme which was also related to preventive measures. It was about the duration of pressure/shear. The first question in this section asked for the reason for repositioning and 35.1% of the participants answered correctly. The second question was concerned with how the occurrence may be reduced and this was answered correctly by 78.1% of respondents . The next was on pressure-reducing mattresses and repositioning and 48.8% got the correct answer. The fourth question on this theme was on the prevention of heel PUs. This was correctly answered by 44.2%. The final question was on PI prevention among bedridden patients and 72.7% got the correct answer. The average percentage level of knowledge in this section was 35.8%.
These tables have presented the overall average score for each question. The majority of the questions were not answered correctly by more than half of the sample population as the level of knowledge was below 50 % in all sections. This indicates a low level of knowledge on PIs and prevention. Further analysis of the data of this study reveals a low level of knowledge on PI prevention. The questionnaire focused on five different themes: aetiology and development, classification and observations of PIs, risk assessment and nutrition about PIs, and preventive measures to reduce the amount and duration of pressure or shear.
In comparison to the results in studies by Barakat-Johnson et al (2018), which was a cross-sectional study conducted in Australia, or to Kopuz et al (2018), a study conducted in Turkey, the level of knowledge on PI prevention shown by Maltese nurses was low. In the descriptive cross-sectional study by Kopuz et al (2018), the mean knowledge score of the population was 52.95 (80.2%) of a possible 66 mark, indicating that the sample population had a higher level of knowledge than that of the present study. In a similar study to Kopuz et al (2018), Barakat-Johnson et al (2018) had a mean knowledge score of 35.21 (74.9%) of a total score of 47. Barakat-Johnson et al (2018) used the Pressure Ulcer Knowledge Test (PUKT) to collect the data while Kopuz et al (2018) used the Information Form and Pressure Ulcer Prevention Knowledge Survey. However, it should be noted that Gedamu et al (2021) stated that when the standard PUKT was used nurses obtained better knowledge scores than when other instruments were used.
Nevertheless, multiple studies indicate a low level of knowledge of PI prevention among nurses. In Sengul et al (2020), a descriptive cross-sectional study conducted in Turkey, only 3.6% (n=17) of the population of 471 nurses were able to score higher than the cut-off point of 60% created by the researcher, and none of the questions of the instrument were correctly answered by the entire sample. Sengul et al (2020) used a Turkish version of the original PUKT. A study that had a result similar to this present study was conducted in Slovakia by Halász et al (2021). Researchers used the PUKT. The results of this quantitative, exploratory cross-sectional study show that there were insufficiencies in the level of knowledge as the population scored only 45.5%. This, however, is still higher than the mean score obtained in the present study (44.6%).
Additionally, in the multi-centre cross-sectional study conducted by Ebi et al (2019) in Ethiopia, only 8.5% of the population (n=18) scored above the average score. Reasons for such levels of knowledge could include, lack of training, heavy workloads, staff shortages, and lack of evidence-based literature (Malinga and Malinga, 2020). In Wu et al (2022), the knowledge score of nurses was 51.5%, while a score of 60% or more indicated a decent level of knowledge. The results, therefore, presented an insufficient level of knowledge. These findings are consistent with those of Jiang et al (2020), where the mean knowledge score was 58.3% and the cut-off point was set at 80%.
Gedamu et al (2021) found an average knowledge score of 46.24% among their participants, which was lower than the cut-off point of 60%, suggesting that nurses working in the hospitals of this review had a low level of knowledge. Furthermore, Emami Zeydi et al (2022), a systematic review set in Iran, also reported an insufficient level of knowledge among Iranian nurses (53.1%), thus failing to reach the cut-off point of 60%, according to PUKAT tools.
Although different studies have found different findings and different levels of knowledge, one should consider that these differences may be related to the data collection tool. Gedamu et al (2021) indicated that the standard PUKAT for data collection obtained a higher level of knowledge than studies that used a standard PU assessment tool. Further research could assess the level of knowledge before and after an educational intervention to determine whether the level of knowledge would have improved. Furthermore, using one standard tool for level of knowledge assessment would make it an easier and more reliable process to replicate and interpret the results of different studies.
The results achieved should not discourage nurses working in an acute hospital in Malta. In-service training, an adjustment of the nursing curriculum with more emphasis on PIs, and an incorporation of the updated guidelines are some suggestions that can improve nurses’ level of knowledge (Ebi et al, 2019). Statistical significance was found in the relationship between the level of knowledge on one hand, and clinical experience and articles read on the other.
The mean score of the perceived barriers was 56.6%. These findings show that nurses working in this hospital perceived more than five barriers, the most common one being lack of staff and workload (95.5%), followed by a shortage of pressure-relieving devices (89.3%)
The number of perceived barriers that these nurses reported to be facing was numerous as well.
Perceived barriers
- Lack of staff or heavy workload
- Poor opportunities to update knowledge
- Lack of guidelines
- Poor risk assessment tools
- Shortage of pressure-relieving devices
- Lack of training
- Lack of job satisfaction
- Lack of multidisciplinary initiative
- Seriously ill patients.
These perceived barriers across socio-demographic data were also assessed and statistical significance was achieved with level of education, clinical experience, source of education, articles read, and training/workshops. Furthermore, a correlation test was used to identify whether there was a relationship between the level of knowledge and the barriers perceived by participants. A weak negative relationship was noted in this study, that is, nurses with a higher level of knowledge had found fewer barriers to implementing PI prevention techniques.
Findings in the context of Benner’s novice to expert theory
The findings are mostly consistent with the theory guiding this study, that proposed by Benner (1982, 1984), which implies that practical experience improves the level of knowledge among nurses. Benner proposes that nurses progress from novice to experts through clinical experience. The findings of this present study indicate that as nurses gain more experience at work, their understanding of and ability to prevent PIs improve. The importance of continuous learning is evident in Benner (1982, 1984), proposing that expertise is related to exposure to real life scenarios and clinical practice and through a progression of the five stages. Each of the stages represents a higher level of skill and comprehension, with ‘novices’ being the nurses with the least experience and ‘experts’ with the most experience and acquiring self-reasoning. In Benner’s theory, clinical experience is a key contributor to the advancement through the five stages. The more years of clinical experiences, the more opportunities for nurses to encounter adverse events, learn from their past experiences and improve their clinical skills. Practical experience develops the intuitive comprehension and clinical reasoning of experts.
Nonetheless, Benner (1982, 1984) believes that although clinical experience is significant for the progression from novice to expert, on its own it does not automatically indicate expertise. Reflection on these adverse events, learning from more skilled professionals, and pursuing more challenges are also components of the theory. This relates to the findings of the present study, where the level of knowledge, although low in novice nurses, did not increase linearly with the number of years of clinical experience.
Limitations and recommendations
This study helped to obtain data on the level of knowledge on PI prevention among nurses working in wards in an acute hospital, thanks to its cross-sectional nature. However, since it was conducted at one point only and limited time was available for the researcher, many factors may have influenced the results. These factors include a lack of focus on the content or an undue haste to finish the questionnaire.
Other designs and methods could be applied to address aims similar to those of the present study. A pre-test and post-test could be conducted to identify any differences in knowledge and perceived barriers before and after a training session or educational seminar. The results would highlight any differences observed and would contribute to the existing literature on the effect of education and training in reducing the development of PIs. A qualitative or mixed-methods study using interviews or focus groups could also present a more in-depth understanding of nurses’ perceived barriers to PI prevention.
Additionally, an observational study would present actual data on how nurses managed PIs and what techniques they implemented to relieve PIs. This would present data based on real observations and the findings could be compared to those of this study to determine any discrepancies between level of knowledge and actual nursing assessment skills. However, an observational study in a hospital setting, raises considerable ethical considerations, especially those concerning patients, and these would have to be addressed.
As observed in the results of this study, the level of knowledge of nurses concerning PIs is low and therefore more education and training is required among nurses on their prevention. Such education should start with the pre-graduate courses, where this topic should be given utmost importance. The issues related to PIs including the length of hospital stays, cost, and the quality of life of patients should be addressed and explained. Student nurses and newly graduated nurses should be allowed to be involved with the tissue viability nurses and in PI management events.
In this respect, the University of Malta has recently offered a Master’s degree course on skin and wound management (Scicluna Ward, 2022). Such courses will certainly improve the level of knowledge among nurses. In addition to official courses by universities, hospital settings should individually provide training and additional educational seminars such as those organised by local associations (Scicluna Ward, 2023) to improve and update the level of knowledge on the latest practices and the proper use of new equipment and dressings. As one of the perceived barriers mentioned by the respondents of this present study was the lack of multidisciplinary initiative, such training should be offered to all members within the team for the benefit of the patient. Nurses should also interest themselves when dealing with PIs.
More education should be given to patients and relatives on the importance of PI prevention (Abela, 2021). The risk factors of the development of PIs should be known. Prevention techniques, such as regular turnings, mobilising if possible and good nutrition and hydration, should be highlighted. Relatives should also be educated on the proper care of PIs upon discharge and the signs of further development of the wound should be clearly explained to avoid potential readmissions to the hospital and the onset of a poor quality of life.
Policymakers and hospital management should prioritise PI prevention. Guidelines and policies should be regularly updated according to the latest research. Perceived barriers, such as those that feature in this study, should be addressed. Increasing staff members, reducing workloads, and providing educational opportunities should be actively considered by hospital managements. The provision of seminars and educational campaigns keep nurses satisfied and happy with their job. A clearer risk assessment tool should be implemented to help nurses manage and decide the best plan of action to prevent or control PI.
Moreover, the lack of availability of pressure-relieving devices should be looked into, and more effort needs to be made to have more of such devices. Training should be held when these devices are made available to nurses. Nurses should also be encouraged to continue their studies in parallel to gaining clinical experience. Nurses assigned with the prevention of PIs should be encouraged to increase their knowledge during their clinical experience and through additional sources of education.
Management and administrations in hospital settings need to focus on continuous professional development and provide opportunities for nurses and other healthcare professionals to update their knowledge of PIs and learn more on the latest techniques and the newest equipment. Hospital management should invest in audits and research and expand one-person PIs teams into full-time interdisciplinary teams. Moreover, PI should be recognised as a quality indicator and be given more attention. Hospitals should also join in the global campaign devoted to an international ‘Stop Pressure Ulcer Day” in November. Continuous education should be mandatory for nurses wishing to remain in the job, as in many other countries. These measures would help to improve nurses’ level of knowledge and decrease the number of barriers that hinder them from performing proper PI prevention.
Conclusion
This research study aimed to identify the level of knowledge and barriers to PI prevention perceived by nurses in the main hospital in Malta. The findings show a low level of knowledge and numerous barriers to prevention perceived by the participants. These factors were observed to be influenced by socio-demographic factors including the nurses’ length of clinical experience and the articles they read. The number of perceived barriers was related to the level of education, clinical experience, source of education, articles read, and training. An increase in the level of knowledge and a decrease in the perceived barriers hindering nurses from performing proper preventive treatment of PIs would improve patient safety considerably and decrease the burden associated with PIs significantly.
What we know:
- PIs represent a prevalent problem in healthcare settings
- A low level of knowledge concerning PI prevention is dangerous as this may affect the well-being of the patients
- Similar to studies in many other countries, a low level of knowledge was found in this research study.
What this study adds:
- This study adds insight into the process of how to assess the nurse’s knowledge in an acute setting
- It provides pragmatic recommendations to the perceived barriers that were evaluated in this research study.
References
