The Meek micrografting technique: clinical applications and outcomes in practice
Received:
Accepted:
Published:
Authors: Erick Zúñiga-Garza, Roger Zambrana-Flores, José Adrián Yamamoto-Moreno, Claudio Daniel Rojas-Gutiérrez, Jorge Said Haro-Cruz, Allan Fernando Delcid-Morazan and Eduardo Camacho-Quintero
Citation:
Zúñiga-Garza E, Zambrana-Flores R, Yamamoto-Moreno FJ et al (2025) The Meek micrografting technique: clinical applications and outcomes in practice. Global Wound Care Journal 1(1): 31-35
Ethical Approval:
All procedures performed in studies involving human participants were in accordance with the ethical standard of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consents:
All patients signed informed consent for surgery, use of photographs and data for publication.
Conflicts of interest:
Eduardo Camacho-Quintero is a member of the editorial board
Corresponding author
Erick Zúñiga-Garza, Av. Félix Cuevas #540 Col Del Valle. Benito Juárez, Mexico City, Mexico. Email: Erickzunigagarza5@gmail.com
DOI: https://doi.org/10.63896/gwcj.1.1.31
Objective: To describe the experience and outcomes of using the Meek micrograft technique in severely burned patients with limited donor areas (n=4) at the National Medical Center “20 de Noviembre”, Mexico City, Mexico.
Methods: A retrospective, descriptive, observational and longitudinal study of four patients with burns >25% of the total body surface area (TBSA) treated with the Meek micrograft technique combined with special dressings (polyurethane foam dressings with silver) was conducted. Variables included age, sex, comorbidities, TBSA, Garcés severity index, aetiological agent, number of interventions, graft integration percentage and epithelialisation.
Results: Four patients of different age groups, with various comorbidities and Garcés severity indices >25%, were included. The average number of surgical interventions was 5.5. The Meek micrograft technique with a 4:1 expansion ratio was used, achieving an average graft integration of 80% at 7 days and 95% epithelialisation at 5 weeks.
Conclusion: The Meek micrograft technique is safe and easy to perform, demonstrating excellent results and advantages over other techniques for skin coverage in patients with burns >25% with limited donor areas. However, it is expensive and not routinely available in Mexican institutions.
The management of patients with major burn injuries remains a challenge for plastic surgeons due to their complexity, lack of donor sites and high mortality rates. Currently, meshed grafts are the workhorse for skin coverage in burn patients.
The surgical principle for treating burn patients consists of debridement and early skin grafts (Janzekovic, 1970). In severely burned patients, large areas of burns cannot be grafted using traditional techniques due to insufficient donor sites (Atiyeh et al, 2005). To address this challenge, multiple techniques have been developed to optimise the grafted skin area, such as meshed grafts and the Meek micrograft technique (Meek, 1958; Atiyeh et al, 2005).
The concept of micrografting was first introduced in 1869 by Jacques-Louis Reverdin, who used it to create small skin islands to promote wound epithelialisation (Hackl et al, 2014). This concept has evolved over time to optimise available donor areas.
Among these techniques, the Meek micrograft technique aims to expand the skin graft based on the principle that the smaller the body, the larger its surface area in relation to its volume. One inch of skin can expand up to 16 inches (Meek, 1958). Dr Parker Meek first performed this technique in 1953, and an article explaining the procedure was published with the title “Forsyth native performs rare skin grafting” (Telegraph News, 1953). While successful, it was difficult to reproduce due to its technical complexity, leading to its overshadowing by the easier-to-reproduce meshed graft technique. However, the meshed graft has limitations concerning donor site/recipient site ratios (Meek, 1958; 1963; Tanner et al, 1964).
With improvements in the survival rates of major burned patients, the scarcity of donor sites has become a limiting factor for achieving skin coverage. Meshed graft techniques require sufficient donor sites and epithelialisation can be delayed with expansions greater than 1:6 (Kreis et al, 1993; 1994).
This study aims to describe the experience and outcomes of the Meek micrograft technique at the National Medical Center “20 de Noviembre” in Mexico City, Mexico.
Methods
A retrospective, descriptive, observational and longitudinal study was conducted by reviewing clinical records from the Department of Plastic and Reconstructive Surgery at the National Medical Center “20 de Noviembre” over a period of 3 years (2020–2022). Patients with burns covering >25% of the total body surface area (TBSA) who underwent skin coverage using the Meek micrograft technique were included. Variables recorded were age, sex, comorbidities, TBSA, Garcés severity index, causative agent, number of interventions, graft integration percentage and epithelialisation at 5 weeks.
Case 1: A 4-year-old male patient was admitted to the burn unit with a diagnosis of scald burn 2 days after the event, with 29% TBSA, including 22% second-degree and 7% third-degree burns on the lower limbs, chest and abdomen. He underwent six surgical interventions, including surgical debridement and the application of polyurethane foam dressings with silver (Mepilex® Ag, Mölnlycke), achieving a small percentage of epithelialisation (10%). Although the patient had low albumin, prealbumin, and transferrin levels, these were normalised through oral nutritional supplements, and subsequently, Meek micrografts were applied in nonepithelialised areas.
Case 2: A 59-year-old female patient was admitted to the burn unit with 30% TBSA burns from deflagration [Figure 1], including 25% second-degree and 5% third-degree burns on the lower limbs. She underwent three surgical interventions, including wound debridement and the application of polyurethane foam dressings with silver (Mepilex Ag) on the first, fourth and tenth days of hospitalisation, followed by Meek micrografts in nonepithelialised areas.

Case 3: A 40-year-old female patient was admitted to the intensive care unit with 41% TBSA burn from deflagration, including deep second-degree burns in the face, lower and upper limbs, and an airway injury confirmed by bronchoscopy. She underwent nine surgical interventions, including wound debridement and the application of polyurethane foam dressings with silver (Mepilex Ag). Meek micrografts were applied to nonepithelialised areas in the final intervention.
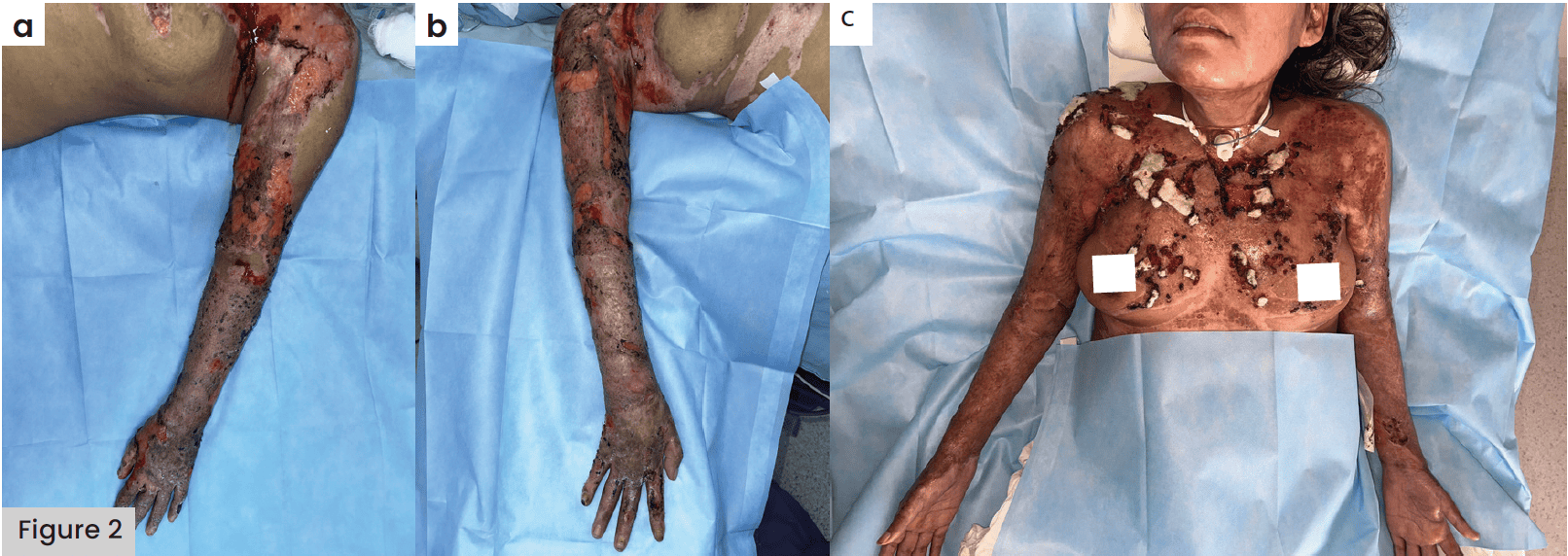
Case 4: A 36-year-old female admitted to the intensive care unit with 30% TBSA burns [Figure 2], including deep second-degree burns in the face, neck, chest, upper limbs and abdomen, she underwent 12 surgical procedures, including wound cleaning, debridement and application of meshed skin grafts, with the loss of these due to infection. Due to an adverse wound bed, we decided to perform skin coverage with micrograft technique in nonepithelised areas.
Description of the technique
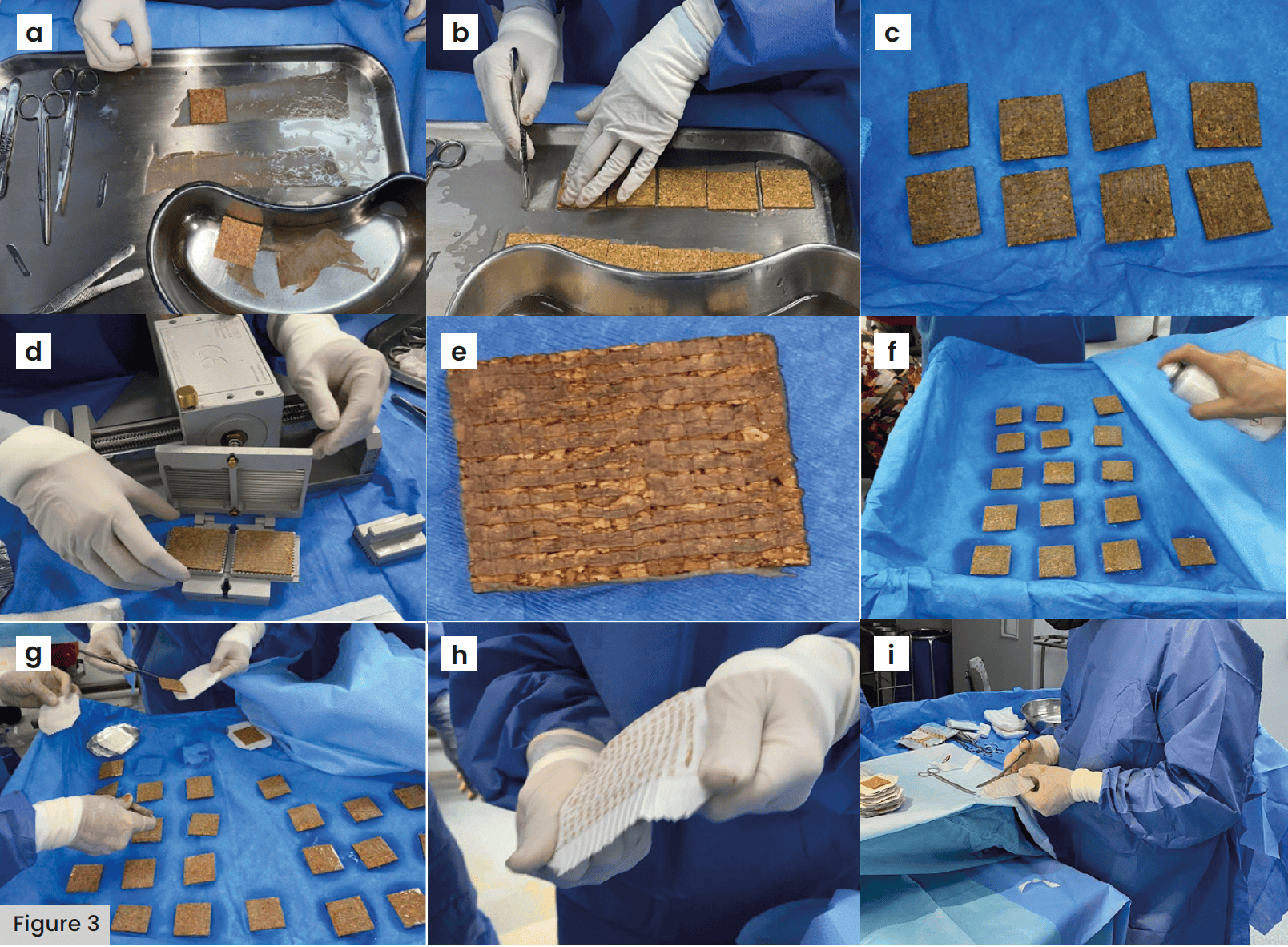
Thin partial-thickness grafts of 0.20 mm with a width of 8 cm and variable lengths (depending on the available donor area) are harvested [Figure 3a]. The burn wound bed is prepared to receive the micrografts. The Meek micrograft technique begins with placing the grafts on corks measuring 42 × 42 mm (with the epidermis facing up) [Figure 3b]. The graft should not exceed the edges of the cork and, if it does, it should be trimmed with a scalpel while maintaining slight pressure on the graft [Figure 3c]. Once the graft is aligned with the cork, it is cut with a dermatome using 13 blades set 3 mm apart in both horizontal and vertical directions [Figure 3d], yielding 196 micrografts [Figure 3e]. An adhesive aerosol is then applied, creating a thin layer on the epidermal side from approximately 30 cm, allowing it to dry for 10 minutes [Figure 3f].
Subsequently, the cork with micrografts is placed in the expansion system with slight pressure, comprising a double layer: first, a fine, folded polyamide gauze of whitish colour, and second, an aluminium sheet that provides firmness and aids in expansion. The expansion system can achieve ratios from 1:2 to 1:16. After 10 minutes, the micrografts adhered to the polyamide gauze are removed from the cork [Figure 3g] and expanded from the centre to the periphery in both longitudinal and transverse directions [Figure 3h]. The aluminium sheet is then removed, and the edges of the polyamide free of grafts are trimmed to facilitate transferring the micrografts to the recipient bed [Figure 3i]. Metal staples are used at four points to secure the grafts, followed by covering them with a secondary nylon fabric dressing coated with metallic silver (Silverlon). The dressings are removed after 7 days, and a protocol of paraffin dressings with chlorhexidine (bactigrass) and residual wound areas with porous collagen membrane dressings (membracel) are used.
Results
Four patients with ≥29% TBSA burns and limited donor sites were included, undergoing harvesting and application of Meek micrografts [Table 1]. The age range was 4–59 years, with one male patient and three female patients. Two patients presented with malnutrition upon admission to our unit, which was normalised through oral nutritional supplements before undergoing the Meek micrografts, and one patient had active smoking.
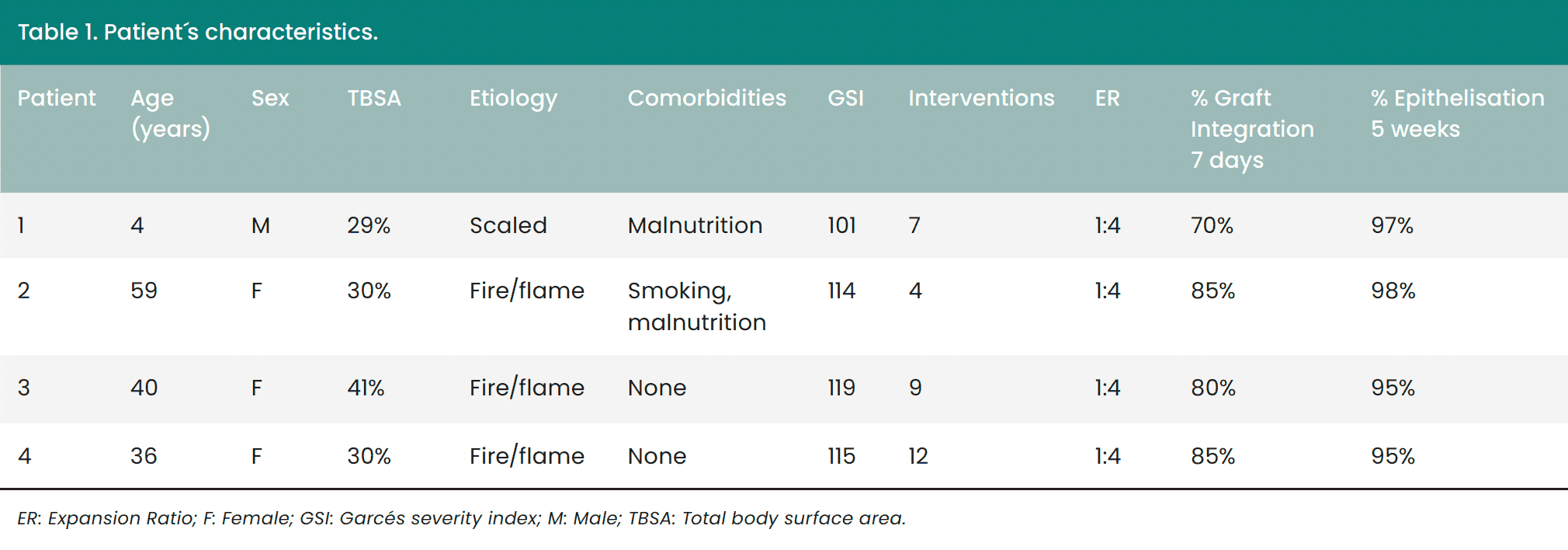
The aetiological agents were: one patient had a scald burn and three had fire/flame burns. The burns were mostly deep second-degree with a small percentage of third-degree burns. The Garcés severity index is an index for mortality prediction in burned patients, and the formula is:
- 40-age of patient + percentage of burn body surface for 1 (superficial), 2 (intermediate) or 3 (full thickness).
The index was over 101 points placing all four patients in group IV (mortality 30-50%).
The expansion ratio of the micrografts were 1:4 for all patients. The time for micrograft integration was 7 days, with an integration percentage of 70%, 85%, 80% and 85%.
The epithelialisation percentage at 5 weeks was nearly 100%, with 97% in the first patient, 98% in the second, 95% in the third and 95% in the fourth.
Discussion
Burns are defined as injuries caused by the acute transfer of energy, generating local zones of hyperaemia, stasis and necrosis, as well as a systemic inflammatory response (Atiyeh et al, 2005; Yakupu et al, 2012). Burns are devastating injuries, often resulting in emotional disorders, decreased quality of life and repercussions on socioeconomic status (Reverdin and Ivy, 1968).
Patients with extensive burns represent a challenge for plastic surgeons due to the large burned areas and limited available donor sites. These patients require a multidisciplinary approach in a burn unit and a surgical team capable of providing adequate skin coverage (Atiyeh et al, 2005).
The principle of burn patient treatment remains that of early surgical debridement and early grafting. Given the conditions of severely burned patients (large affected areas, limited donor sites), the Meek micrograft technique offers a solution by allowing greater skin expansion than traditional meshed grafts (Atiyeh et al, 2005; Meek, 1958; 1963).
In wounds with micrografts, epithelialisation is driven by the proliferation and migration of keratinocytes. Micrografts (0.8 × 0.8 mm) initially survive by diffusion of wound fluids, supported by the wound’s microenvironment (Quintero et al, 2018). Micrografts proliferate independently of their orientation, contributing to wound epithelialisation (Benmeir et al, 1991).
In 1958, Meek described his original technique to maximise graft area by passing the graft through a 13-blade electric cutter, placing it on flat cork plates described as “carriers,” these microdermagrafts were manually transferred and saturated in plasma and evenly distributed to prefold parachute silk bandages, which were placed directly on the wound bed (Meek, 1958).
Due to the technical difficulties of the Meek micrograft technique, meshed grafts became popular due to their easy application and consequent reduction in surgical time. However, the difficulty of handling expansions greater than 1:4, the need for abundant donor area, and the requirement of an optimal surgical bed highlighted the limitations for skin coverage in patients with major burns using this technique (Kreis et al, 1993; 1994).
In 1993, a modification of the original technique was described, with the addition of a special adhesive to secure the grafts to the cork plates and pre-folded nylon. These modifications simplified the reproduction and acceptance of the technique for treating burn patients (Kreis et al, 1994).
Similarly, the tissue expansion capacity was compared for each technique. The Meek micrograft technique achieved an expansion rate of 1:9 with a maximum distance between skin islands of 8-9 mm, while the meshed graft technique achieved an expansion rate of 1:6 with a distance between skin elements of 11-12 mm, resulting in faster epithelialisation between grafts with the Meek micrograft technique. Skin islands are not connected, so the loss of some does not result in a significant loss of the graft, whereas in a meshed graft, the loss of a small area can result in a large segment loss (Kreis et al, 1993; 1994).
Another advantage of the Meek micrograft technique is the maximum optimisation of skin fragments used on the cork, avoiding waste of any fragment, even small islands of 1 or 2 mm, which is not possible with the traditional meshed graft technique (Benmeir et al, 1991).
Integration and epithelialisation are higher with the Meek micrograft technique in suboptimal conditions compared to meshed grafts in the same situations (Benmeir et al, 1991; Wang et al, 2006). In our study, some patients had comorbidities and high mortality yet achieved epithelialisation of ≥95% at 5 weeks.
Post-integration management with special dressings is important. In our study, paraffin dressings with chlorhexidine were used to cover micrografts, aiming for mechanical protection, preventing desiccation and overgranulation tissue growth, allowing for edge-to-edge progress between micrografts and adequate epithelialisation (Benmeir et al, 1991; Quintero et al, 2018).
It has been demonstrated that hospital stay, and epithelialisation time are shorter with the Meek micrograft technique (Wang et al, 2006), which was also evident in our patients with an epithelialisation rate of nearly 100% at 5 weeks.
Cosmetic advantages have been reported in patients undergoing Meek micrografts, presenting a more uniform, smooth and flexible grafted surface compared to meshed grafts (Munasinghe et al, 2016; Hsieh et al, 2008), which is relevant due to the predisposition of these patients to pathological scarring.
The disadvantage of this technique is the limited availability and high cost of the equipment required. The “20 de Noviembre” National Medical Center is a referral institution in Mexico with a burn unit, thus having a multidisciplinary team and the necessary resources for managing great burned patients.
In our experience, we encountered some technical issues that can be avoided, such as adhesive contact with the meshes (separating meshing and adhesive application areas on different surgical tables or using surgical drapes to cover meshing), applying the spray adhesive generously to ensure the epidermal layer adheres well to the dressing, preventing micrografts from losing orientation during expansion, and trimming edges of dressings free of micrografts to improve alignment and coverage in difficult-to-access areas like joints.
Conclusion
The modified Meek micrograft technique is an alternative for skin coverage in major burned patients (>25% TBSA) in whom a characteristic is the limited availability of donor areas. This technique, compared to traditional meshed grafting, presents multiple advantages, is reproducible in any age group, offers a greater expansion range and adequate integration, and is well-tolerated in nonfavourable conditions for graft integration.
References:
