Primary care nurses’ knowledge and attitudes towards the management and prevention of diabetic foot ulcers
Received:
Accepted:
Published:
Authors: Rachel Faenza, Professor Cynthia Formosa, Corinne Scicluna Ward
Citation:
Faenza R, Formosa C, Scicluna Ward C (2025) Primary care nurses’ knowledge and attitudes towards the management and prevention of diabetic foot ulcers. Global Wound Care Journal 1(2): 52–60
Conflicts of interest:
CSW is on the Global Wound Care Journal editorial board; this did not influence acceptance.
Corresponding author
Corinne Scicluna Ward, Faculty of Health Sciences, University of Malta, Tal-Qroqq, Msida, MSD 2080, Malta. Email: corinne.scicluna@um.edu.mt
DOI: https://doi.org/10.63896/gwcj.1.2.52
Background: Nurses working in primary care are well positioned to be key health care professionals to prevent and manage diabetic foot ulceration (DFU). They play a crucial role in identifying and managing predisposing factors of DFU. Thus, having sound knowledge about DFU care and a positive attitude towards these patients is very important in promoting patient-centred care.
Aim: To evaluate primary care nurses’ knowledge and attitudes towards the management and prevention of DFU in the primary healthcare centres in Malta.
Design: A cross-sectional design was selected.
Method: An online questionnaire was distributed to all nurses who work in wound care clinics within the primary health care centres in Malta (n=105). A total of 50 questionnaires were returned generating a response rate of 48%.
Results: The results showed that primary care nurses had a suboptimal knowledge of DFU management and prevention, with an average score of 57.38%. No significant relationship was found between knowledge scores and sociodemographic factors. While nurses had an overall positive attitude toward DFU care, with a mean score of 79.5%, some negative attitudes were noted, including concerns about the time-consuming nature of DFU care and the inability to educate every patient on prevention. There was a significant correlation between positive attitudes and interest in DFU care (p=0.005), as well as between knowledge and attitude scores (p=0.006).
Conclusion: This study highlights that primary care nurse have suboptimal knowledge about management and prevention of DFU, however, an overall positive attitude towards care for patients with DFU. More specialised training courses offered to nurses on a continuous basis are needed to ensure optimal quality of care towards patients with diabetes. Nurses should be given an incentive to attend these courses to develop their skills, keep abreast with evidence-based practices and optimise the provision of care.
This study aims to assess primary care nurses’ knowledge and attitudes toward managing and preventing diabetic foot ulceration (DFU). Diabetic foot ulcers (DFUs) are serious complications of diabetes, contributing to hospitalisations, amputations and even death (Armstrong et al, 2017). Predisposing factors include diabetic neuropathy, peripheral artery disease (PAD), trauma and infection (Malhotra et al, 2012). Diabetic patients are at an increased risk of developing foot infections due to neuropathy, PAD and a weakened immune system (Noor et al, 2017). Osteomyelitis also raises the risk of antibiotic failure, leading to lower-limb amputation (Kosinski and Lipsky, 2010).
Proper management can delay or prevent major DFU complications (National Institute for Health and Care Excellence [NICE], 2019). However, inadequate knowledge among interdisciplinary teams can result in diabetic patients receiving insufficient guidance on ulcer care (Canadian Diabetes Association Clinical Practice Guidelines Expert Committee and Cheng, 2013). Attitudes toward care are also crucial, as nurses’ perceptions influence the holistic management of chronic wounds (Kumarasinghe et al, 2018). Primary care nurses play an essential role as first points of contact for patients and their families (Vargas et al, 2017). Marques et al (2019) highlighted the importance of nurses in providing health education, follow-up care and promoting self-care routines. Additionally, Corbett (2012) stresses that nurses should receive objective education on wound management and be empowered in their roles within the healthcare team.
Theoretical framework
The theory of planned behavior (TPB), first discussed by Ajzen in 1985 (Ajzen and Madden, 1986) and further developed in 1991 (Ajzen, 1991), was used in this study to explore the relationship between background factors and nurses’ attitudes towards DFU care. According to TPB, an individual’s intention to perform a behaviour is influenced by their attitude, subjective norms and perceived control over factors that may facilitate or hinder the behaviour (Ajzen, 2011). This study aimed to examine how factors such as age, experience, education and exposure to information influence nurses’ attitudes towards caring for patients with DFU. Additionally, a secondary aim was to investigate the relationship between knowledge and attitudes as informed by the TPB that suggests that knowledge can impact attitude.
Methods
Study design and setting
A cross-sectional survey was conducted with a random sampling approach in primary health care centres. This comprised nine independent centres covering the north, central and south area of the island of Malta. Quantitative research was chosen as it provides a numerical description of trends, attitudes or opinions of a given population (Creswell and Creswell, 2017). Moreover, a cross-sectional approach was chosen as data could be collected at one point in time and opinions or attitudes collected from one specific group of individuals (Edmonds and Kennedy, 2016). Since the researcher had a limited amount of time to conduct the study, a self-administered online questionnaire was deemed appropriate and provided anonymity that could help decrease desirability bias which happens during interviews when participants answer in a certain way to please the researcher rather than being truthful.
Additionally, as Carbonaro and Bainbridge (2000) state, online data collection methods have several advantages, including the relatively short time to collect data and the fact that the data are less likely to be lost and easier to be transferred into a data programme for analysis. However, online questionnaires have disadvantages with the main one being the low response rate, and this may be due to the individual’s interest or his/her perceived relevance of the survey (Carbonaro and Bainbridge, 2000). To limit these disadvantages and increase the response rate, the researcher sent multiple reminders to the participants and targeted a population of nurses who were most likely to see relevance in the topic as they were directly involved in caring for patients with DFU regularly.
Target population and sampling procedure
The inclusion criteria for this study included Nurses with at least 1 year of experience and who work in wound care clinics within the primary healthcare centres The researcher contacted the Human Resources office of primary care to identify the number of the nurses working in the health centres of Malta. A total of 300 nurses were identified, however, this included nurses who also worked in other areas apart from the wound care clinics. Hence, convenience sampling was implemented to collect data only from the nurses who worked in wound care clinics. Convenience sampling is used when the researcher wants to obtain the most accessible sample population that will reflect the inclusion and exclusion criteria (LoBiondo-Wood and Haber, 2006).
Thus, in this study, the charge nurse of every health centre was approached and asked to provide the number of nurses who work in wound care clinics who fell in the stipulated criteria. A total number of 105 nurses was identified. The required sample size was calculated using the online “surveysystem” calculator which is used by researchers to obtain appropriate sample size. Through a maximum margin of error of 5%, and a 80% degree of confidence, a sample of 65 participants was generated.
Ethical clearance was obtained from the Faculty Research Ethics Committee (FREC), University of Malta. The DPO forwarded a Google Forms link to eligible participants, with an information letter provided at the start of the questionnaire. Google Forms was considered an adequate and secure platform for administering the survey, as no personal identifiers or GDPR-sensitive information were collected. Access to the collected data was restricted, with only the principal researcher holding the account credentials. The platform’s built-in encryption and access controls were deemed sufficient for the nature of the data gathered. Participants were informed that participation was voluntary and they could withdraw at any time. As the questionnaire was anonymous, written consent was not required and completion of the form implied consent. Anonymity and confidentiality were ensured, with no personal or identifying details collected. Based on a 5% margin of error and an 80% confidence level, the required sample size was calculated to be 65 participants for adequate statistical power. However, after the data collection period ended, a total of 50 participants were recruited in this study.
Data collection tool
The “Questionnaire on Assessment of Nurses’ Knowledge and Attitudes on Diabetic Ulcers,” originally developed by Kumarasinghe et al (2018) was utilised in this study. This tool measured the knowledge and attitude variables for the prevention of the DFU.
Demographical data were eventually adjusted for the purpose of the local study. The next section consisted of questions about their knowledge on DFU and the questions were divided in three subcategories: Predisposing factors and ulcer characteristics, ulcer complications and diabetic ulcer care. The categories related to the nurse’ attitude were made up of four components: lack of care for people with diabetic ulcers (questions 2, 7, 8, 9), denial of diabetic ulcer care (questions 10, 11), diabetic ulcer care (questions 1, 3, 4) and priority in diabetic ulcer care (questions 5, 6).
A Likert-type scale with four responses options was used. The statements in the questionnaire where purposefully negatively worded by the creator of the tool. This means that the best positive attitude was shown when the answer was strongly disagree and the least positive attitude was shown when the answer was strongly agree. In 2023, this tool was tested again for validity and reliability by Sarmiento-Luna et al. and obtained a Cronbach’s Alpha coefficient of 0.84 for the knowledge subscale and of 0.62 for the attitude subscale (Sarmiento-Luna et al, 2023). Permission was sought and granted by the authors prior to data collection.
Data collection and analysis
To enhance the response rate, participants were sent a reminder email 2 weeks after the initial invitation, followed by a second reminder 2 weeks later. The data were extracted from Google Forms and inputted into Excel, then coded numerically. Descriptive and statistical analyses were performed using SPSS version 21®. The correlation between knowledge scores and positive attitude towards DFU care was also sought. The Pearson correlation coefficient was used to investigate whether a relationship between knowledge and positive attitude scores is significant or not.
One-way ANOVA testing was used to examine relationships between variables.
Results
Sociodemographic data and DFU knowledge characteristics
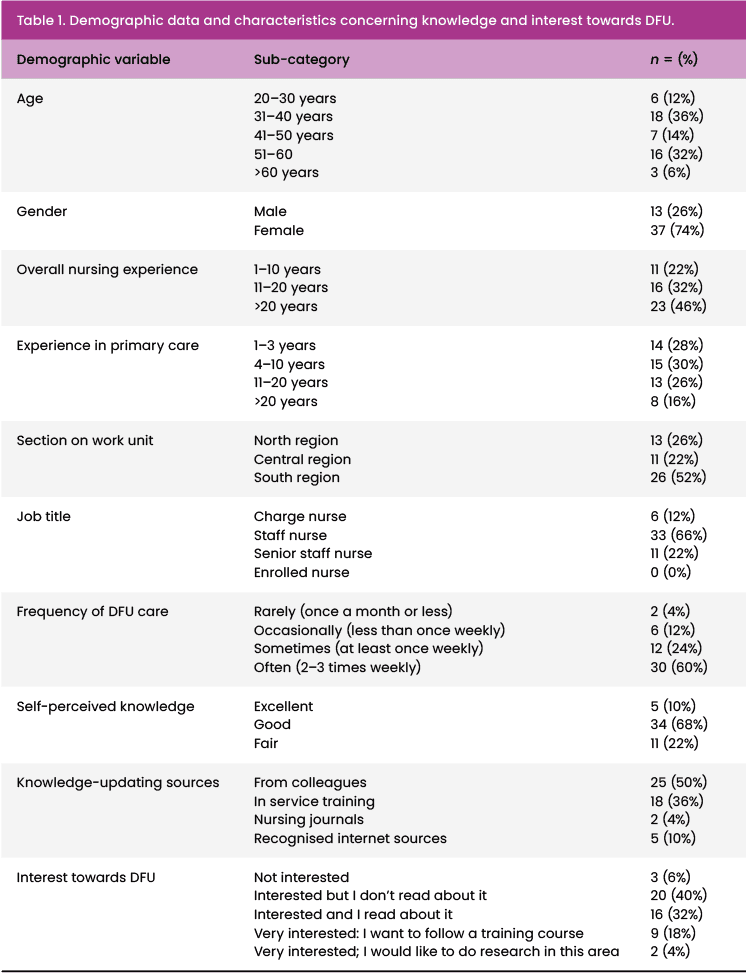
Table 1 outlines the sociodemographic and DFU knowledge characteristics. The majority of participants were female, aged between 30 and 60, with 78% (n=39) having over 11 years of nursing experience. The difference between a nurse and a senior nurse is the number of years plus the degree/diploma they hold. According to the sectoral agreement (2023) page 14: “A Staff Nurse/Psychiatric Mental Health Nurse, with an appropriate Masters’ Degree at MQF level 7 or PhD at MQF level 8, shall undertake a competency programme and evaluation framework. Upon successful completion of the competency programme and evaluation framework, and subject to satisfactory performance, a Staff Nurse/Psychiatric Mental Health Nurse (with Masters/PhD) with at least two (2) years of satisfactory service as Staff Nurse/Psychiatric Mental Health Nurse in Salary Scale 8, shall be promoted to the grade of Senior Staff Nurse/Senior Psychiatric Mental Health Nurse in Salary Scale 8, and to Salary Scale 7 after three (3) years of satisfactory service in the grade of Senior Staff Nurse.”
Regarding DFU care, Table 1 presents the relevant findings. Notably, in terms of self assessed knowledge, most nurses rated their knowledge of DFU as good (68%, n=34) with only 10% (n=5) rating it as excellent. Notwithstanding this, only 32% (n=16) were both interested and read on the topic and only 18% (n=9) were very interested in attending a training course.
The results for the knowledge scores indicate that nurses performed well in the subcategory of ‘Predisposing factors and ulcer characteristics’, with almost all participants answering correctly. However, they scored poorly in the other two subcategories. In the ‘Ulcer complications’ subcategory, which included three questions, over half of the nurses answered two out of three questions incorrectly. Specifically, 66% (n=33) incorrectly answered that neuropathic ulcers cause pain and 78% (n=39) incorrectly answered whether the presence of slough indicates infection.
In the ‘Diabetic ulcer care’ subcategory, nurses also scored poorly, with most answering three out of four questions incorrectly. For example, 82% (n=41) incorrectly answered whether neuropathy is manifested by cold skin and reduced pulses, while 86% (n=43) answered incorrectly regarding the recommendation of hyperbaric therapy for a well-perfused limb. Additionally, 72% (n=36) incorrectly responded to the question about using iodine dressing to control infection.
The overall knowledge mean score for primary care nurses was 57.38%. When analysing the subcategories individually, nurses scored well in ‘Predisposing factors and ulcer characteristics’ (mean score: 80.75%), but scored poorly in both ‘Ulcer complications’ (mean score: 34.5%) and ‘Diabetic ulcer care’ (mean score: 33.5%).
Statistical analysis using one-way ANOVA showed no significant relationship between sociodemographic variables or other characteristics of interest and knowledge scores.
Data analysis for attitude scores
Table 2 illustrates how the nurses answered when asked questions about their attitudes towards DFU.
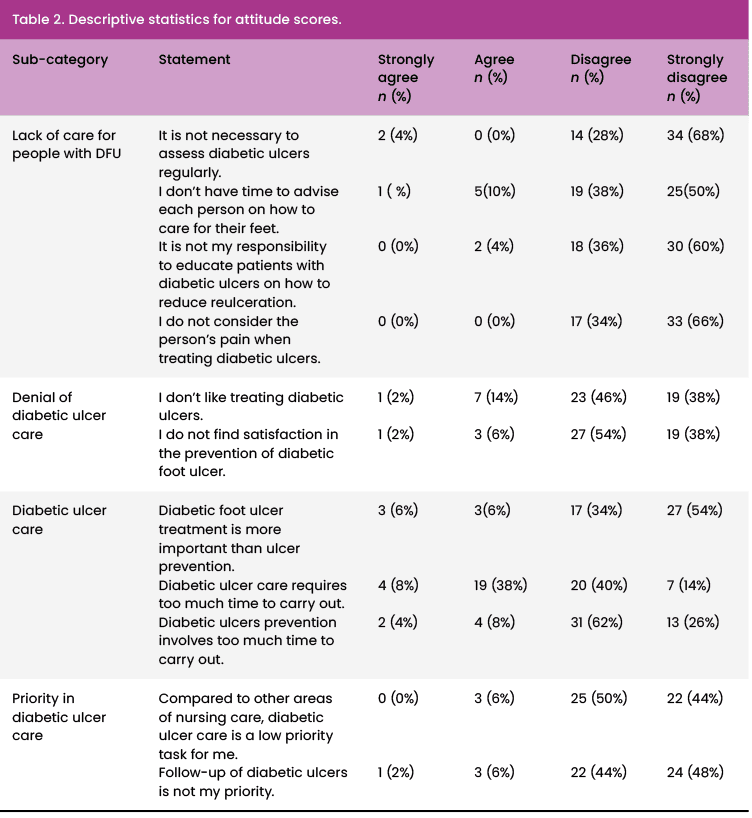
Table 2 shows that most nurses answered strongly disagree or disagree in most of the statements. This shows that overall, the nurses’ attitudes towards the care of DFU are very positive. However, it can be noted that some of the nurses had negative attitudes in relation to prevention and time management of DFU care. The highest percentage of negative attitude was 38% where 19 nurses agreed that DFU care takes too much time to undertake. Fourteen per cent (n=7) of nurses also reported that they did not like to treat diabetic ulcers and 10% (n=5) reported that they did not have time to advise each patient about foot care.
The participants scored an overall mean percentage score of 79.5%. In all the subscales, there was an evident positive attitude with the highest being in the subscale named “Lack of care for people with DFU” with a score of 87.25%. Following the statistical analysis with the one-way ANOVA parametric test, only one statistically significant difference was identified between the positive knowledge scores and the interest towards DFU (p= 0.005). In fact, a positive relationship was found between the level of interest towards DFU and positive attitude scores(p=0.005).
There is also a positive relationship between the level of interest and positive attitude towards DFU care. Nurses who showed interest and wanted to follow a training course had a higher mean percentage score (91.41%; n=9) than the nurses who were interested but did not read about it (74.77%; n=20).
There is a strong statistical significance between the sub-category of “denial of diabetic ulcer care”, (p<0.001), where nurses who were interested and did not read about DFU reported a less-positive attitude score (71.88%; n=20) than those nurses who were interested and read about it (83.59%; n=16) and those who are interested and want to follow a training course (87.5%; n=2).
Correlations between the knowledge about DFU and positive attitude scores
The results show a positive correlation between knowledge and positive attitude scores which is statistically significant and not attributed to chance with a p-value of 0.006.
Discussion
This study investigated the level of knowledge and attitudes that nurses have towards caring for patients with DFU. TPB was used as a framework to understand the attitude of primary care nurses.
The results revealed that nurses demonstrated good knowledge of neuropathic ulcers, with an average score of 80.75% for correct answers. However, their understanding of managing ulcer complications and preventive care was lacking, with mean scores of 34.5% and 33.5%, respectively. This is concerning, as these nurses care for diabetic patients and should be knowledgeable about ulcer complications and prevention. Early detection of complications is crucial for timely intervention and appropriate wound care, which can prevent ulcer progression and reduce the risk of amputation (NICE, 2019). Additionally, 40% of participants (n=20) were unaware that epithelisation is linked to healing progress and 82% (n=41) did not recognise the manifestations of neuropathy. Consequently, the overall knowledge score was 57.38%.
Although the findings of this study indicate that nurses possess suboptimal knowledge regarding DFU care, consistent with previous research (Bilal et al, 2018; Kumarasinghe et al, 2018), some contextual differences should be considered. In these international studies, the majority of participants held only diploma-level qualifications, whereas in the present study, nearly half of the nurses (48%, n=24) had attained either a bachelor’s or master’s degree. Moreover, while nurses in the previous studies had an average of 5 to 10 years of professional experience, a substantial proportion of participants in this current study (78%, n=39) had over 11 years of nursing experience. Given these demographic differences, comparisons may be more appropriately drawn with studies such as those by Kaya and Karaka (2018), Alkhatieb et al. (2022) and Abdullah et al (2017), where participants similarly held higher academic qualifications and had between 6 to 16 years of experience.
Notably, those studies reported a higher level of DFU-related knowledge among nurses. Therefore, the finding that knowledge remains suboptimal in the current cohort — despite their educational background and experience — raises concerns and warrants further investigation into potential gaps in training, continuing education or institutional support for DFU care.
This study examined the relationship between sociodemographic factors, experience, education and self-perceived knowledge with actual knowledge scores in the care of DFUs among nurses working in PHC in Malta. No significant correlation was found between years of experience (overall or in primary care) and knowledge scores, consistent with previous studies (Ng et al, 2020; Alkhatieb et al, 2022; Abdullah et al, 2017; Sharmisthas et al, 2013), but contradicting findings by Kumarasinghe et al (2018) and Bilal et al (2018), who reported a significant relationship. Similarly, the level of education did not show a significant link to knowledge scores, which aligns with Abdullah et al (2017).
Interestingly, nurses with a nursing certificate, despite having lower educational levels, scored the highest in knowledge, likely due to greater experience. From these results it is important to consider that there was no clear link between nurses’ education level or years of experience and their actual knowledge of DFU care. This is not something expected because one assumes that more education or experience would lead to better knowledge. Interestingly, nurses with only a certificate qualification scored the highest, possibly because of hands-on experience. This suggests that formal education alone may not be enough, and that practical training or exposure to DFU care could play a bigger role. It also raises questions about whether current nursing education and ongoing training are effectively covering this important area of care.
These results are also interesting when put into context with other results from the study that found 68% of the nurses rated their self-perceived knowledge as “good,” though their actual knowledge scores varied, with many nurses scoring low. There was a positive trend between self-rated and actual knowledge, but it was not statistically significant, as seen in Albagawi et al (2023). Concerning knowledge sources, half of the nurses relied on colleagues for updates, with limited participation in formal education activities such as in-service training or journal articles, which aligns with Kumarasinghe et al (2018) and Bilal et al (2018). A lack of incentives for further education and specialisation was identified as a key issue, as continuous training is not mandatory in Malta.
Additionally, nurses’ interest in DFU care was positively related to their knowledge scores, consistent with Kaya and Karaka (2018). Nurses who showed an interest in DFU care, through reading or attending training, had higher knowledge scores, supporting findings from Felix et al (2021) and Ramzan et al (2022). The study calls for specialised, continuous training courses for nurses with incentives to encourage participation and for more specialised nurses to monitor DFU care and standardise practices.
The study’s second aim was to assess nurses’ attitudes toward DFU care using TPB (Ajzen, 2005), which posits that positive attitudes lead to positive behaviours. The findings showed that nurses had a generally positive attitude toward DFU prevention, with a mean score of 79.5%. However, while overall attitudes were positive, some negative views were observed, particularly regarding the time-consuming nature of DFU care. This finding aligns with studies by Kumarasinghe et al (2018), Bilal et al (2018), and Ng et al (2020), who also reported similar results. A finding that is concerning is the high percentage of negative attitude (38%, n=19) when nurses agreed that DFU care takes too much time to carry out.
Overall, these results show a significant number of nurses expressing a reluctance to spend time advising each patient, which is concerning given that proper foot care advice can prevent 85% of amputations (Khatib and Malazy, 2007). However, it can be postulated that a possible reason for this response is the heavy workload which nurses encounter which in return leaves insufficient time for nurses to provide holistic care to every patient. In fact, lack of time and lack of staff were found to be potential barriers in a study evaluating barriers towards pressure ulcers prevention (Moore and Price, 2004).
Notwithstanding these results, this study found very positive attitudes regarding the regular assessment of DFU and considering the patient’s pain during treatment. It was found that the Maltese results contrasted with previous international studies by Kumarasinghe et al (2018) and Bilal et al (2018) who found insensitivity to pain as a common negative attitude. Another positive and encouraging finding related to the education of patients on how to avoid reulceration, Nearly all nurses in the study disagreed that they were not responsible for patient education, a finding that contradicted Kaya and Karaca (2018) and Alkhatieb et al (2022), who reported low levels of patient education.
The study explored relationships between attitude scores and sociodemographic factors (age, education level and years of experience), finding no significant links between attitudes and most factors. However, older nurses (over 60) had more positive attitudes than younger nurses (20-30), and more experienced nurses also showed slightly better attitudes. These results align with Tubaishat et al (2013), who found a positive relationship between experience and attitude towards DFU prevention. Education level, however, showed no significant correlation, consistent with Moore and Price (2004) and Etafa et al (2018), who also found no link between attitude and educational level. While this study found no significant overall relationship between nurses’ attitudes and most sociodemographic factors, the trend of more positive attitudes among older and more experienced nurses is worth noting. This may suggest that attitudes toward DFU care improve with time and practical exposure, rather than through formal education. The lack of association between education level and attitude, consistent with previous studies, (Moore and Price, 2004; Etafa et al, 2018) raises concerns about whether current nursing programmes effectively influence or shape professional attitudes toward chronic wound care. It also suggests that experience on the job may have a stronger impact on attitude development than academic qualifications alone.
This study also revealed that nurses who expressed a stronger interest in DFU care tended to have more positive attitudes toward its management. More specifically, nurses who read about DFU or showed interest in the subject displayed more positive attitudes, implying that better knowledge contributed to a better attitude towards the care of patients with DFU. This was statistically significant (P=0.005) and mirrored findings by Kumarasinghe et al (2018), who also found that interest in DFU care was linked to more positive attitudes. Nurses who read about DFU had higher positive attitude scores than those who did not, supporting the TPB’s assertion that exposure to information influences attitudes (Ajzen, 2005). Thus, this study recommends that nurses be encouraged to engage with current research on DFU, with clinical guidelines and up-to-date wound care protocols made easily accessible in treatment areas.
According to TPB, factors such as skills, abilities and knowledge can influence behaviour (Ajzen and Madden, 1986). The results of the study showed a statistically significant positive correlation between nurses’ knowledge and their positive attitudes (p=0.006), contradicting findings from studies by Kumarasinghe et al (2018) and Bilal et al (2018), which found no correlation between knowledge and attitude scores. However, the findings were similar to Abdullah et al (2017), who observed a moderate positive correlation between knowledge and practice scores, and Beeckman et al (2011), who found a correlation between knowledge and attitude regarding pressure ulcers.
The study concluded that higher knowledge about DFU was associated with more positive attitudes towards caring for DFU patients, suggesting that nurses’ knowledge influences their attitudes. As per Fishbein and Ajzen (2005), individuals are more likely to act positively when they feel they have the knowledge and resources to do so. Although actual behaviours were not observed in this study, it can be inferred that nurses with positive attitudes are more likely to engage in positive behaviours, potentially leading to better nursing care. The study recommends further research, including observational and qualitative studies, to explore if nurses’ attitudes are reflected in their behaviours.
Study limitations
The study utilised TPB to interpret the results and understand the relationship between nurses’ attitudes and background factors. However, TPB assumes that attitudes predict behaviour, but as the study did not observe actual behaviours, it was not able to analyse how nurses’ attitudes translated into practice. Moreover, not all the criteria and items of the TPB were explored. More time would have been useful to conduct further research through an observational study to evaluate the actual behaviour and practice of nurses.
Lastly, social desirability bias is a concern as nurses may have over-reported positive attitudes toward DFU care, skewing the results toward socially acceptable responses (Anvari et al, 2022). Although this study revealed that nurses generally have overall positive attitudes, results should be taken with caution due to the possibility of over-reporting responses where nurses could have answered positively as this is more socially acceptable. Further research which may include observational and qualitative studies is recommended to understand nurse’s actual behaviour towards DFU and to establish if their attitude reflects their behaviour (Anvari et al, 2022).
Conclusion
In conclusion, this study provided valuable insights into the knowledge and attitudes of primary care nurses regarding DFU management and prevention. A notable knowledge gap was identified, particularly concerning ulcer complications and ulcer care. While nurses generally exhibited positive attitudes, some negative views were noted, especially regarding the time and effort allocated to ulcer care and education. A positive relationship between nurses’ knowledge and attitudes was found, suggesting that enhancing knowledge could lead to better attitudes and, ultimately, improved patient care.
The study highlights the need for continuous specialised training in DFU management for nurses. Regular educational programmes, alongside the recruitment of more nurses trained in wound care and the establishment of tissue viability clinics in primary care, could further incentivise nurses to deepen their expertise. Additionally, further research in this area is necessary to ensure that patients with DFU receive optimal care and that nurses are well-equipped to manage this condition effectively
